Veterinary Advice: Vaccination Failure - When Vaccines Don't Seem to Work.
Vaccines are products containing minimally harmful viral or bacterial antigens
(surface proteins and sugars) similar to those contained on the surfaces of wild-type
infectious-disease-causing organisms which, when administered to an animal, are designed to induce a protective
immune system response against disease-causing organisms that might infect that animal.
Sometimes, however, despite our best efforts, a vaccinated animal will develop
signs of the disease that we are trying to protect it from. This is termed
vaccination failure
or
failure of immunization.
Generally, it occurs because of one of two reasons:
1) The clinical disease is being caused by the vaccine itself (live vaccines only) OR
2) The clinical disease is being caused by a wild-type, infectious disease organism
that has infected the animal from its local environment.

Clinical disease caused by the vaccine:
Live vaccines are functional, replicating strains of the exact same viruses and
bacteria that we are trying to protect our pets from. They only differ from the wild-type disease causing agents in that they been specially 'bred' and selected for their
avirulent properties (e.g. they might not replicate as quickly as the wild viruses or
they might not access the host's cells as well). Consequently, when live vaccines are
manufactured and used correctly, it is very unlikely that they should ever cause disease
in a normal animal with a normal immune system (even a naive immune system which has not
yet been exposed to the vaccine viruses, like that found in our puppies at first vaccination)
In some cases, however, live avirulent vaccines can cause the diseases they are trying
to prevent. This happens for the following reasons:
1) There has been a failure of quality control at the manufacturer and a virulent strain
of virus has made it into the vaccine.
The effect of injecting a virulent strain of
virus (e.g. parvo, distemper) is the same as if you had just taken a small puppy
and let it lick up the poo from a dog with parvo! The animal will develop disease
because its immune system is naive and not able to cope with the virulence of the virus strain.
2) The vaccine was given by the wrong route.
The most notable occasion when this happens
is with the injectable cat-flu vaccines. Live, injectable cat-flu vaccines are often
moderately virulent strains of virus. The main reason they do not normally induce
disease is that they are inoculated at a site that they do not normally grow well in
(under the skin). If, however, they are accidentally inhaled (this can occur when a vaccine
is drawn up and aerosolized in the cat's presence), they will get access
to the cells of the respiratory tract (which is their preferred site for replicating
and causing disease). Cat-flu will result with all of the sneezing, fever, eye discharge
and nasal discharge associated with the condition.
3) Mild clinical disease is a known side effect of the vaccine route.
Sometimes, mild signs of the disease are common and accepted side effects of the vaccine. This is particularly true of the intranasal vaccines (kennel cough and cat flu intranasal spray vaccines): animals will often get mild signs of coughing, sneezing
and watery eye and nose discharges after these vaccines. It is also a known side effect of the feline calicivirus injectable (sometimes kittens will show lameness
and fever after vaccination, a condition sometimes seen in the calicivirus disease).
Generally, these mild side effects are self-limiting and do not need medication.
4) Vaccination of the pregnant animal with a live virus vaccine.
Foetuses are unprotected against live vaccine
viruses (their immune systems are very immature) and many of the organisms will
preferentially replicate in the rapidly-dividing cells of the foetus. Damage to
fetal cells can result in stillbirths, abortion, fetal abnormalities or puppies and
kittens born with clinical disease. Well known examples of this: fetal kittens whose
mother received a live panleukopenia vaccine can be born showing signs of an
underdeveloped cerebellum (they will tremor whenever they move).
 5) Vaccination of neonatal (newly born) puppies and kittens that did not get their
colostrum with a live vaccine.
5) Vaccination of neonatal (newly born) puppies and kittens that did not get their
colostrum with a live vaccine.
Although live vaccines are fine for use
in animals over 4 weeks old (which have a functional, though naive immune system) and newborn animals
protected by their mother's colostrum, newborn animals (termed neonates) unprotected by maternal antibodies have a greatly reduced immune response (not much better than the late-stage fetus) and live vaccines may produce disease in them.
6) Vaccination of animals with a poor immune system.
Although live vaccines are
not as virulent as wild-type vaccines, they do replicate in cells and damage them
(it just takes them longer). By the time they grow numerous enough to do any real harm,
the immune system has generally come along to kill them off, thereby preventing vaccine-associated
disease and acquiring the needed immunity. If, however, the immune system response fails to 'show up', the live vaccine viruses will continue to replicate as the wild-types do
and they will eventually produce symptoms of disease.
Situations where animals might have a poor immune system:
- Animals born with a bad immune system.
Some purebred dogs and cats (and other species) have a genetic predisposition to immunodeficiency (they lack parts of their immune system).
An example of this is CID (Combined ImmunoDeficiency) in Arabian horses. These foals are
born with non-functional T cells and, as a result,
not only do their T cells not work, but their B cells also can not be activated to make
antibodies (immature B cells initially need T cells to activate them). They suffer from
a lack of both humoral and cell-mediated immunity (see How Vaccines Work page for details on what these terms mean). Live vaccines would induce disease in these animals
and they often die young from overwhelming infection - they essentially have no immune system.
- Animals that acquired a bad immune system.
There are many diseases and drugs which
damage (permanently or transiently) the immune system, making it inadequate to fight off wild-type diseases and live vaccine organisms. These include:
A) Radiation therapy - can destroy the bone marrow which makes most of the white cells.
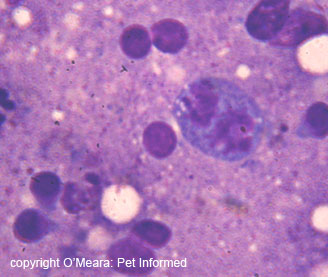
B) Bone-marrow-invasive disease - diseases such as leukemia (bone marrow cancer
can invade and destroy the bone marrow so that white blood cells can't be made.
C) Bone-marrow-suppressive drugs - some medications stop the bone marrow making white cells. These include most chemotherapy drugs (e.g. vincristine, azathioprine, cyclophosphamide),
corticosteroids (e.g. prednisolone) and long-term estrogen products in dogs (normally used to treat incontinence).
It is a reason we don't vaccinate dogs on immune suppressive drugs such as prednisolone.
D) Auto-immune diseases that kill the white blood cells in the blood or the cells in the bone-marrow that make them.
E) Viral diseases - FIV in cats (feline AIDS) kills off many of the T cells. Feline
leukemia virus can result in auto-immune diseases (point D) and leukemia (point B).
Canine and feline parvoviruses also damage the bone marrow during clinical illness (note that a veterinarian would never vaccinate a dog or cat this unwell).
F) Bone marrow suppression can occur in undesexed female ferrets (they get estrogen poisoning).
This is why vets recommend desexing female ferrets.
- There are also some situations where the condition of the animal may induce hormonal
and chemical changes in its body that might result in a poor immune system response and
a potential for vaccine-induced disease signs. These include:
A) Excessive stress (including pregnancy) - natural cortisols produced during times of excessive, prolonged stress (we are not talking about the otherwise well, shivering chihuahua sitting on the consult table) will suppress the immune response to vaccination.
B) Very old animals - over time and age, the immune system of most animals starts to
deteriorate. This can result in a subnormal immune response.
C) Fever - certain elements of the immune system do not work as effectively during
times of high body temperature.
D) Subnormal temperatures - as with fever, some immune cells do not work as well
when body temperatures are very low. It would be rare for vets to vaccinate a cold animal,
however, one situation in which this could occur is when vaccines are given to animals
that are under anaesthesia.
E) Severely malnourished animals - animals need nutrition for immune cells to replicate
and for antibodies to be made.
Unwell animals that are already relatively immunosuppressed because their immune system
is invested in fighting another disease process can potentially develop vaccine-associated
infections with live vaccines. The fact is, there are not enough immune cells to go around! Vaccination of unwell animals can result in live vaccines causing disease (e.g. dogs infected with nasty, wild-type parvo virus that are then vaccinated against distemper have been known to develop clinical distemper from the vaccine!). It can also
result in the pre-existing disease becoming worse (white blood cells abandon the initial area of disease to 'fight the vaccine', resulting in the initial disease
becoming more severe). It is for this reason that vets do not vaccinate sick animals.

Clinical disease being caused by a wild-type, infectious disease organism even though the animal is vaccinated:
Generally, if a cat or dog (or other animal) has been vaccinated in accordance with
vaccine company recommendations (vaccine schedules) and has been isolated appropriately from
other animals and public areas until it is deemed protected, it is very unusual for these animals to ever be infected with or to show clinical of disease from
encounters with these infectious organisms in the environment.
Sometimes it occurs though and 'apparently protected' animals will become infected
by and show disease from wild-type viruses and bacteria. This occurs for many reasons,
which can be divided into: Testing factors, Patient (host) factors, Vaccine and
procedural factors and Disease (virus/bacteria) factors.
Testing factors:
False positive test results.
Sometimes an animal will test positive (especially in in-house
vet test kits) for a disease that it has been vaccinated against, but hasn't actually got.
Confused? I'll use some commonly-encountered examples to explain:
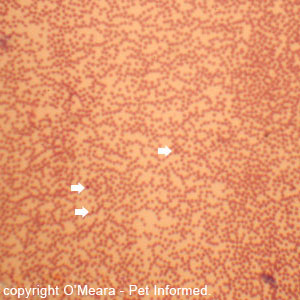
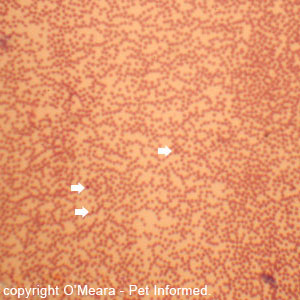
Common example 1: any young dog that comes into a vet clinic with vomiting, diarrhea (especially if there is blood in the diarrhea) and general unwellness will be
tested for parvo virus. The dog could have any number of diseases - we are not yet
sure it is parvo. In this test, a swab of feces is taken from the dog's bottom
and run through a test kit to see if it contains parvo virus antigens (these are
proteins or sugars on the surface of the virus that are specific to parvoviruses).
If the test comes up positive, we say that the dog has parvo. Right? Well, sometimes. False positives: if a dog has been vaccinated with a live parvo vaccine 4-14 days
before the test was run, the animal will shed vaccine-associated parvovirus antigens
into its feces and these will yield a positive result on the fecal test! So, an animal
that is vaccinated and protected against parvo will appear to have been infected with
the disease!
Common example 2: when we vaccinate cats for FIV, the cats will produce antibodies
against the FIV vaccine in their blood (see the How Do Vaccines Work page for more details).
These will hopefully protect the cat against infection with the real FIV virus. The trouble is
that the test we use to detect a cat with true FIV (the disease) is an antibody-detection
test. Both cats with real, disease-type FIV and cats that have had the FIV vaccine (and which should be protected against the disease) will test positive! It is for this reason
that vets will microchip all cats that they give the FIV vaccine to: shelters that pick up stray cats will test them for FIV and, if they do not have a chip, they will euthanase
these cats.
Common example 3: The test for Lyme disease in animals can sometimes produce false positives
in animals that do not have Lyme disease, but some other inflammatory disease such as polyarthritis or SLE (systemic lupus erythematosis).

Patient (host) factors:
This normally boils down to the fact that, for some reason, this animal was incapable of mounting a normal, protective immune response to the vaccine organism and, consequently, was left unprotected against the real thing. Many of these factors are the exact same as those described in the above section on live vaccine-induced disease.
1) Vaccination of animals with a poor immune system.
In addition to being susceptible to
disease from live vaccines, animals with a poor immune system may not be capable of mounting an effective, protective immune system response towards vaccination
(e.g. killed, not live, vaccines might be tried in them). This would leave them open to environmental disease organisms. These animals include:
- animals with congenital immune defects (they were born with them)
- animals with acquired drug-induced, cancer-induced, infection-induced and auto-immune-induced immunodeficiencies.
- very old and very young animals (poorer immune system responsiveness)
- very unwell animals (the immune system is either suppressed or invested elsewhere
in fighting off other disease)
- the very malnourished (you need nutrition to make cells and antibodies)
- very stressed animals (this includes pregnancy stress). Stress increases the levels
of cortisol (a glucocorticoid or corticosteroid) in the blood which suppresses
the immune system.
- febrile animals (fever alters the immune cell responses)
- hypothermia / subnormal temperature: (certain immune system cells don't work
as well when the body is cold.)
To use one common example: animals with black and tan coloration (dobermanns, rottweilers
and mastiff/Staffordshire bull terrier types) have always been considered more prone to
parvovirus infection than other breeds. Vets have even resorted to 2-weekly vaccine protocols
and vaccinations up to 20 weeks of age to try to protect them. Some will still get parvo
regardless. The assumption is made that either their immune system is particularly poor
at inducing a preventative immune response towards this virus or their maternal immunity
(see point 4) lasts an inordinately long time.
2) Vaccination (esp live organism inoculations) causes relative immune suppression.
When a
vaccine is given (esp a live vaccine, which replicates in the body) lots of white blood
cells get mobilised to try and kill it. This results in a relative deficiency of white blood cells being available to defend the body against other diseases that might come along.
Consequently, recently vaccinated animals are more prone to infection with infectious
organisms, including the nasty, wild-type viruses and bacteria that we are trying
to prevent with vaccination.
3) The host was already infected with a wild-type disease-causing organism when it
was vaccinated. As a result, not only is this animal not yet protected by the vaccination, but
the immunosuppressive effects (see point 2, above) of the live vaccine (occ killed vaccine)
might even cause the wild-type infection to become more severe!
4) Puppies and kittens with prolonged maternal immunity.
 The main reason most puppies and kittens do not die of infectious disease shortly after birth is that most of them drink their mother's colostrum (also called first milk). Colostrum contains antibodies against the major infectious disease organisms that have been encountered by the bitch /queen in her
environment in the past (including the live or killed organisms that the mother encountered during vaccination). These antibodies (termed maternal immunity) enter the blood
of the puppies or kittens and circulate there for up to 14 weeks, defending the young animals from infection (see How Vaccinations Work section for info on what antibodies do). It is a great system because it keeps the young animals alive while their immune systems are maturing.
The main reason most puppies and kittens do not die of infectious disease shortly after birth is that most of them drink their mother's colostrum (also called first milk). Colostrum contains antibodies against the major infectious disease organisms that have been encountered by the bitch /queen in her
environment in the past (including the live or killed organisms that the mother encountered during vaccination). These antibodies (termed maternal immunity) enter the blood
of the puppies or kittens and circulate there for up to 14 weeks, defending the young animals from infection (see How Vaccinations Work section for info on what antibodies do). It is a great system because it keeps the young animals alive while their immune systems are maturing.
The trouble comes when we vaccinate. When we vaccinate, we are giving the pup a tiny dose of a minimally-harmful (avirulent) live virus or bacteria. We want the pup's immune system to be exposed to this organism and to attack it so that, in the future, if the pup is exposed to a nasty wild-type environmental form of the organism its immune system will recognise it and act quickly to neutralise it, thereby preventing
disease. The issue with maternal antibodies is that they are able to attack and neutralise our vaccinated viruses very quickly, thereby preventing the pup from being exposed to them and gaining protective immunity.
If the maternal immunity is only short-lived and wears off after 6-8 weeks, then there won't be a problem: the pup will be exposed to and mount a response to a 10 or 12 week vaccine, if not the initial 6-8 week one (see vaccine schedules page). But if the maternal immunity is really strong (high levels of long-lasting antibody), it could remain in the pup for up to 14 weeks. If only a 6-8 week, (occ an additional 10 week) and 12 week vaccination
was given, all of these could potentially be rendered useless by maternal immunity, leaving the pup unprotected.
Note that newer vaccines have been designed to overcome the issue of maternal immunity and so vaccine failure for this reason should become rarer.
5) Some forms of vaccine-acquired immunity are naturally incomplete and/or short-lasting.
Vaccinations
against the infectious respiratory disease pathogens (feline rhinotracheitis (herpesvirus), feline
calicivirus, feline chlamydia, Bordetella bronchiseptica, canine parainfluenza)
are never considered 100% effective in preventing disease. Even vaccination with
intranasal vaccines (see bottom of how vaccines work page for advantages of intranasal vaccines), though more effective than injectable respiratory virus vaccines, is not 100% preventative.
e.g. vaccinating your dog against kennel cough will not prevent kennel cough if your dog happens to encounter
a dog that coughs virus all over it.
The failure of 100% protection is for many reasons, the main one being the fact that, as with human flu vaccinations,
the strains of feline and canine respiratory viruses are altering all the time from
season to season. Viruses mutate constantly. The production of new vaccines to account for the new strains will always lag behind the appearance of the new strain in the environment. The best that we can hope for when vaccinating against the respiratory viruses is
that signs of infection, if they should appear, will be much milder than they would have been had the animal been unvaccinated.

Vaccine and Procedural Factors.
Failure of vaccination can occur because of the innate limitations of the vaccine itself or
because the vaccine was either not given properly or stored properly (making it ineffective)
or because the animal was allowed to be exposed to infection before the vaccine has had time to have effect.
1)The vaccine was not stored properly.
Vaccines, particularly the live vaccines which
contain live organisms, are very sensitive to storage conditions. They can not be
allowed to get too hot or too cold or come into contact with ice-packs etc. If they do,
the vaccine can die and, thus, it will not be effective inducing protective immunity.
2) The vaccine was given past its use-by-date.
The use-by-date is the date the vaccine should be considered reliable to according to vaccine company studies. Live attenuated vaccines, in particular, should be considered to have a finite lifespan
(the lifespan of the live organisms), after which the vet might simply end up inoculating
useless, dead organisms into the animal.
3) The vaccine was not injected within a certain period of time after reconstitution.
When a vaccine arrives at a vet, it is usually in a powered, dried form that needs to
be mixed in a diluent before injection. If the vet makes up the vaccine (mixes it
in diluent) and leaves it sitting on a bench or in a fridge for more than a couple of hours,
the vaccine will become inactive and ineffective at inducing immunity.
4) The vaccine was not given according to company vaccine recommendations
(vaccine guidelines).
All vaccines are thoroughly tested by vaccine makers during
production and, as a result of this testing, the manufacturers come up with a list of vaccine protocols and recommendations by which the vaccine should be given if it is to achieve its best effect.
These might be important guidelines designed to overcome maternal immunity; important protocols designed to
achieve a stronger, longer duration immune response (e.g. you need a minimum of at least two doses of a killed vaccine to achieve the desired response) or important protocols
designed to reduce the risk of vaccine side effects. If the vet does not follow these
company guidelines and administer the vaccine according to the schedules set out
by the company, the animal may not be protected adequately against disease.
This also applies to timing of boosters. Vaccines do not provide indefinite protection
and booster vaccinations are needed to provide ongoing cover.
 5) Disinfecting the skin with alcohol or antiseptics can potentially render the vaccine ineffective. Sterilising syringes and needles can also leave residues that
may kill off the vaccine organisms.
5) Disinfecting the skin with alcohol or antiseptics can potentially render the vaccine ineffective. Sterilising syringes and needles can also leave residues that
may kill off the vaccine organisms.
6) Certain types of vaccines are less effective at inducing a protective immune
response than others.
Generally live vaccines induce a much stronger and longer-lasting
duration of cell-mediated and humoral immunity than killed vaccines do. This is discussed in the live and killed vaccines section of the How Vaccinations Work
page.
7) The puppy or kitten was exposed to wild-type infectious disease organisms before
it was fully protected by the vaccines.
It takes time for vaccines to induce
a protective immune response in a young animal. The time taken varies according to
the individual type of vaccine, with some vaccines only achieving full protection
after a course of 2-3 injections has been completed and other vaccines (e.g. some of the newer Fort Dodge and Intervet vaccines) giving full cover within a week of
just a single dose (e.g. Nobivac DHP and DuramuneAdult C3) or within three days of an intranasal vaccine (e.g. Nobivac KC).
The consequence of this is that, even though your puppy or kitten might have been given a needle recently by your vet, this does not mean that it is protected and that
it is yet ready to meet other dogs and cats or walk in public places (which could
be contaminated with diseases).
A major cause of vaccine failure is taking pups and kittens out to meet with other
animals before they are fully protected. Be sure to ask your veterinarian when
puppies and kittens can start socializing safely.
Another potential risk is bringing diseases home with you. If you have visited a place where there has been a parvovirus infection or an outbreak of kennel cough or cat flu, don't bring these diseases back to your house where your unprotected puppy or kitten
can catch them! Change your clothes, disinfect your shoes (with parvo, this disinfection
requires powerful chemical virucides like bleach) and shower thoroughly (including washing your hair)
before greeting your pet. Ideally, disinfection should take place somewhere other than
your own home. The same precautions should be taken when other people visit your home:
ask them if they have had any potential contact with infectious diseases.
Note - the issue of time taken to achieve protection is important to consider
when getting a pet vaccinated for kennels or a cattery. It is no good remembering to vaccinate
your pet a day before it is due to go in! The animal will not be covered and the kennel or cattery
(if it is a responsible business) will not accept its admission.

Infectious organism factors (virus, bacteria factors).
1) The strain of infectious disease organism.
Over time, environmental bacteria and viruses mutate, changing in their virulence (ability to cause severe disease) and in the structure
of their surface antigens (the bits that the protective immune system response induced by vaccination needs to recognise in order to kill the organisms - see how do vaccines work page). Sometimes
these wild-type, disease-causing strains differ enough from the viruses / bacteria contained in the vaccines that, despite vaccination, the animal is not protected against them.
 For example, over recent decades a new strain of parvovirus (termed the 2b strain) has appeared (we have seen it in Australia) which does not appear to be fully
protected against by some vaccines. Fully-immunized dogs, sometimes more than
6 months in age, can develop full-blown parvo as a result of this organism and some may
even die. Note - Fort Dodge has produced a range of vaccines (including the new three-yearly DuramuneAdult C3 vaccine) which include protection against this strain of parvovirus.
For example, over recent decades a new strain of parvovirus (termed the 2b strain) has appeared (we have seen it in Australia) which does not appear to be fully
protected against by some vaccines. Fully-immunized dogs, sometimes more than
6 months in age, can develop full-blown parvo as a result of this organism and some may
even die. Note - Fort Dodge has produced a range of vaccines (including the new three-yearly DuramuneAdult C3 vaccine) which include protection against this strain of parvovirus.
2) Animal was exposed to a high viral or bacterial load (i.e. the animal received
a massive 'dosage' of infectious organisms).
Any animal, even animals that have been
fully vaccinated, can develop clinical disease from a vaccinated-against pathogen
if they are exposed to massive amount of the organism. Certain levels of infection can simply overwhelm the immune system so much that clinical disease is experienced.

To go from this Vaccination Failure page to the Homepage, click here.

References and Suggested Readings:
1) Prevention of Infectious Diseases. In Nelson RW, Couto CG, editors: Small Animal Internal Medicine, Sydney, 1998, Mosby Inc.
2) Greene CE, Immunoprophylaxis. In Greene CE, editor: Infectious Diseases of the Dog and Cat, St. Louis, 2006, Saunders Elsevier.
3) Greene CE, Canine Viral Enteritis. In Greene CE, editor: Infectious Diseases of the Dog and Cat, St. Louis, 2006, Saunders Elsevier.
4) Resistance of the Body to Infection: II. Immunity and Allergy. In Guyton AC, Hall JE, editors: Textbook of Medical Physiology, Philadelphia, 1996, WB Saunders Company.
5) Wolf AM, Other Feline Viral Diseases. In Ettinger SJ, Feldman EC, editors: Textbook of Veterinary
Internal Medicine, Sydney, 2000, WB Saunders Company.
6) Hoskins JD, Canine Viral Diseases. In Ettinger SJ, Feldman EC, editors: Textbook of Veterinary
Internal Medicine, Sydney, 2000, WB Saunders Company.
7) Information on DuramuneAdult C3 taken from information provided by Fort Dodge Australia Pty Limited, 2007.
8) Information on Nobivac DHP and Nobivac KC taken from information provided by Intervet Australia Pty Limited, 2007.

Pet Informed is not in any way affiliated with any of the companies whose products
appear in images or information contained within this article. The images, taken by Pet Informed, are only used in order to illustrate certain points being made in the article.
Copyright March 2008, www.pet-informed-veterinary-advice-online.com.
All rights reserved, protected under Australian copyright. No images or graphics on this Pet Informed website may be used without written permission of their owner, Dr. O'Meara BVSc (Hon).
Duramune, Protech and Fort Dodge are registered trademarks of Wyeth and its affiliates.
Nobivac is a registered trademark of Intervet.
Any dose rates mentioned on these pages should be confirmed by a vet. Dosing rates for common
drugs are being changed and updated all the time (e.g. as new research comes in and as drug
formulations change) and information here may not remain current for long. What's more, although we try very hard to maintain the accuracy of our information, typos and oversights do occur. Please check with your vet before dosing any pet any medication or drug.
 The main reason most puppies and kittens do not die of infectious disease shortly after birth is that most of them drink their mother's colostrum (also called first milk). Colostrum contains antibodies against the major infectious disease organisms that have been encountered by the bitch /queen in her
environment in the past (including the live or killed organisms that the mother encountered during vaccination). These antibodies (termed maternal immunity) enter the blood
of the puppies or kittens and circulate there for up to 14 weeks, defending the young animals from infection (see How Vaccinations Work section for info on what antibodies do). It is a great system because it keeps the young animals alive while their immune systems are maturing.
The main reason most puppies and kittens do not die of infectious disease shortly after birth is that most of them drink their mother's colostrum (also called first milk). Colostrum contains antibodies against the major infectious disease organisms that have been encountered by the bitch /queen in her
environment in the past (including the live or killed organisms that the mother encountered during vaccination). These antibodies (termed maternal immunity) enter the blood
of the puppies or kittens and circulate there for up to 14 weeks, defending the young animals from infection (see How Vaccinations Work section for info on what antibodies do). It is a great system because it keeps the young animals alive while their immune systems are maturing. 5) Vaccination of neonatal (newly born) puppies and kittens that did not get their
colostrum with a live vaccine.
5) Vaccination of neonatal (newly born) puppies and kittens that did not get their
colostrum with a live vaccine. 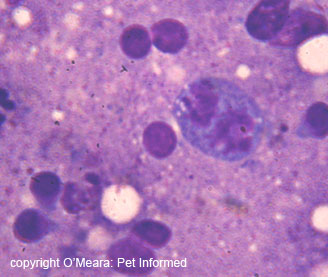
 5) Disinfecting the skin with alcohol or antiseptics can potentially render the vaccine ineffective. Sterilising syringes and needles can also leave residues that
may kill off the vaccine organisms.
5) Disinfecting the skin with alcohol or antiseptics can potentially render the vaccine ineffective. Sterilising syringes and needles can also leave residues that
may kill off the vaccine organisms.  For example, over recent decades a new strain of parvovirus (termed the 2b strain) has appeared (we have seen it in Australia) which does not appear to be fully
protected against by some vaccines. Fully-immunized dogs, sometimes more than
6 months in age, can develop full-blown parvo as a result of this organism and some may
even die. Note - Fort Dodge has produced a range of vaccines (including the new three-yearly DuramuneAdult C3 vaccine) which include protection against this strain of parvovirus.
For example, over recent decades a new strain of parvovirus (termed the 2b strain) has appeared (we have seen it in Australia) which does not appear to be fully
protected against by some vaccines. Fully-immunized dogs, sometimes more than
6 months in age, can develop full-blown parvo as a result of this organism and some may
even die. Note - Fort Dodge has produced a range of vaccines (including the new three-yearly DuramuneAdult C3 vaccine) which include protection against this strain of parvovirus.