Veterinary Advice Online - Coccidia Infection. Coccidiosis in dogs, cats and other animals.
 Coccidia is a general term for a range of microscopic protozoan parasites that inhabit
the intestines and, occasionally, other bodily organs of animals and humans. The
information contained within this page provides information and advice on the common intestinal coccidian species (Isospora, Hammondia, Besnoitia and Sarcocystis) known to cause gastrointestinal disease, enteritis and symptoms of weight loss, dehydration, diarrhea, mucoid and bloody feces, straining to defecate and, occasionally, vomiting in puppies and kittens. If your vet has performed a fecal float on the faeces of your kitten or puppy and diagnosed your pet with coccidia or coccidiosis - this is the page for you.
Coccidia is a general term for a range of microscopic protozoan parasites that inhabit
the intestines and, occasionally, other bodily organs of animals and humans. The
information contained within this page provides information and advice on the common intestinal coccidian species (Isospora, Hammondia, Besnoitia and Sarcocystis) known to cause gastrointestinal disease, enteritis and symptoms of weight loss, dehydration, diarrhea, mucoid and bloody feces, straining to defecate and, occasionally, vomiting in puppies and kittens. If your vet has performed a fecal float on the faeces of your kitten or puppy and diagnosed your pet with coccidia or coccidiosis - this is the page for you.
The information presented in this page is detailed (but still easy to understand) because we are
aiming to educate owners thoroughly about the disease, including its transmission, symptoms, treatment
and prevention, and provide owners with enough information that they might be better informed and able to troubleshoot problems with their own pets.
Coccidia Contents
1) What is coccidiosis? - a basic overview of the disease and its symptoms.
2) Which animals are at risk of contracting coccidia?
2a) Coccidia in dogs and cats.
2b) Coccidia in livestock and poultry.
2c) Coccidia in wildlife, including Australian wildlife.
2d) Coccidia in people. Is the disease contagious (zoonotic) to man?
3) How do animals contract coccidia? - this section contains information about where and how animals (focus is on dogs and cats) catch coccidia and the roles that stress and environmental factors play in the disease.
3a) Coccidia transmission (includes info on wildlife and livestock reservoirs of coccidia).
3b) What environmental conditions predispose to coccidia transmission and manifestation of disease symptoms?.
3c) Real-life situations that promote dog to dog and cat to cat transmission of coccidia.
3d) My pet hasn't been near another dog or cat in months - how could he get coccidia?
4) Symptoms of coccidiosis in dogs and cats - what does coccidia do to your dog or cat? This section contains the following subsections:
4a) How coccidian parasites cause disease (how they replicate and destroy cells etc.).
4b) Symptoms of coccidia: how do coccidia affect the gastrointestinal tract?
Section includes information on
coccidial symptoms and secondary coccidial complications: dehydration, blood loss, secondary bacterial infections, intussusception, rectal prolapse and fading kittens and puppies. Contains great veterinary medical pictures.
4c) Chronic, recurrent coccidia infections - coccidia that keeps coming back.
4d) Coccidia diagnosed in adult dogs and cats - is it significant?
4e) Can animals be infected with coccidia and show little or no signs of disease?
4f) Sarcocystis neurona (equine protozoal encephalomyelitis), a newly emerging, feline coccidian disease.
5) How is coccidiosis diagnosed?
5a) Fecal flotation.
5b) Fecal smears.
5c) Fecal oocyst culture for sporulation.
5d) Intestinal biopsies.
5e) Additional diagnostics - when you are not certain coccidia is to blame.
6) What other diseases look like coccidiosis in cats and dogs?
7) Coccidiosis treatment
7a) Antimicrobials - coccidiostatic drugs.
7b) Antibiotics - antibacterial drugs.
7c) Intravenous fluids.
7d) Blood transfusions.
7e) Dietary support.
8) What is the prognosis for coccidiosis in canines and felines?
9) How to prevent coccidia in pets. - this section contains excellent general advice on the prevention of coccidiosis for pet owners.
10) How to prevent coccidiosis in high risk situations. - this section contains useful tips and hints
for preventing and controlling coccidiosis infection and spread in situations with high parasite contamination
and high dog and cat numbers (e.g. breeding facilities, pet shops, boarding kennels, vet clinics).
11) How do you disinfect the environment following feline and canine coccidia contamination?
12) How do you disinfect/decontaminate coccidia-infected meat?
13) Summary and take home messages - a summary of the important points.
Please note that other closely-related, highly problematic coccidian species such as Neospora, Toxoplasma and Cryptosporidium will not be discussed here - they will shortly have their own specially dedicated
pages.
WARNING - IN THE INTERESTS OF PROVIDING YOU WITH COMPLETE AND DETAILED INFORMATION, THIS SITE DOES CONTAIN MEDICAL AND SURGICAL IMAGES THAT MAY DISTURB SOME READERS.

1. What is coccidia infection (coccidiosis)?
Coccidia are microscopic protozoan parasites that infest and damage the cells lining the
intestinal walls (small intestine and sometimes large intestine) of kittens and puppies and, occasionally, adult dogs and cats. There are many species of protozoan parasite that come under the general heading of
'coccidia' and which may be able to cause disease in animals. The common dog and cat species
include: Isospora (Isospora canis, I. burrowsi, I. ohioensis and I. neorivolta in the dog and Isospora felis and I. rivolta in the cat);
Hammondia; Besnoitia (cat only) and Sarcocystis. Wild animals (e.g. opossums, kangaroos, wallabies, birds) and livestock (e.g. calves, piglets, poultry) have their own coccidian parasite species, including: Eimeria, Sarcocystis and certain Isospora species.
No mention will be made of the closely-related intestinal protozoan parasite species: Neospora, Toxoplasma and Cryptosporidium as these organisms create very different disease syndromes with different presentations and significance to animals and humans.
The disease, coccidiosis, is contracted when kittens and puppies (cats and dogs) consume feces, faecally-contaminated soil and vegetation and (depending on the parasite species involved) the uncooked meat and organs of rodents and other wild and livestock animals, which are contaminated with
infectious coccidian organisms. The infestation that results causes damage to the lining of
the small intestine, and occasionally the colon, sometimes resulting in symptoms of intestinal and colonic upset. Coccidiosis is a multifactorial disease in that the appearance of disease symptoms
depends not only on the presence of infectious organisms (coccidia), but on other, non-organism
factors including stress, host immune system integrity, the age of the animal host and a wide
range of contributing environmental factors (e.g. overcrowding of animals, poor sanitation).
Section 3 has plenty of excellent information on environmental and host factors contributing to coccidia disease presentation.
Animals that do develop symptoms of disease may present with variable degrees of: inappetence; dehydration; abdominal pain; weight-loss; mucoid, slimy (jelly-like) faeces; putrid-smelling faeces; fresh, bright red blood in the faeces; watery to mucoid diarrhea and repeated straining to defecate.
Vomiting can sometimes occur, but is a less-common finding. Most dogs and cats that
present with clinical signs of coccidiosis are under 4 months of age (although older animals
can sometimes become symptomatically affected). Most of these affected animals
are bright and alert, despite their symptoms, and often recover without complication. Kittens and puppies can, however, sometimes become very sick from the disease (due to severe dehydration, blood loss or secondary bacterial infection and complications) and may even die without prompt and proper therapy.

2. Which animals are at risk of contracting coccidia?
2a) Dogs and Cats:
Dogs and cats - definitive hosts:
 Dogs and cats of any age are able to ingest infectious coccidian parasites and have them
replicate within their intestinal tracts. Whether or not this coccidian infection actually results in any symptoms of disease (diarrhoea etc.), however, has a lot to do with
the age and immune system integrity of the animal host. Coccidian oocysts (the infectious
parasitic cysts shed in the host-animal's faeces) can often be found in the feces of older cats and dogs without these animals showing any signs of disease. Typically, coccidiosis disease symptoms are only seen
in very young puppies and kittens (under 4 months old) whose immune systems are not
yet mature enough to manage and control the parasitic invaders.
Dogs and cats of any age are able to ingest infectious coccidian parasites and have them
replicate within their intestinal tracts. Whether or not this coccidian infection actually results in any symptoms of disease (diarrhoea etc.), however, has a lot to do with
the age and immune system integrity of the animal host. Coccidian oocysts (the infectious
parasitic cysts shed in the host-animal's faeces) can often be found in the feces of older cats and dogs without these animals showing any signs of disease. Typically, coccidiosis disease symptoms are only seen
in very young puppies and kittens (under 4 months old) whose immune systems are not
yet mature enough to manage and control the parasitic invaders.
The kittens and puppies with the most severe infestations of coccidia (most severe signs of disease) are often those with histories of poor living conditions (e.g. poor sanitation, squalid housing) and/or high stress-levels (stress further suppresses the host immune system). Kittens and puppies that are thin and malnourished; have other intestinal diseases (e.g. parasites and worms); are living in overcrowded conditions (lots of disease spread) or that are living in
conditions of poor sanitation and poor husbandry (extremes of heat and cold, draughts, lots of underweight kittens and puppies all walking around in each other's feces etc.) are most likely to suffer from the disease. Sometimes, just the stress of moving to a new home can be
enough to bring out the disease symptoms in a young animal (e.g. bringing a kitten home from a shelter
or pet shop can be enough stress to make it display disease symptoms). Occasionally, older dogs and cats can display symptoms of coccidiosis if placed under conditions
of high stress or if they develop other intestinal diseases or immune system suppressive disorders (e.g. cats that
catch FIV, animals on chemotherapy or immune suppressant drugs). Animals with congenital
immune disorders are prone to severe, recurrent coccidial infestations - this may be
a reason why the German Shepherd breed is thought to be particularly prone to this parasite.
Some terminology and parasite pointers:
Because these aforementioned coccidial species (Isospora, Hammondia, Besnoitia and Sarcocystis) are able to replicate within the intestines of the dog or cat, achieve sexual maturity
in these hosts and create infectious cysts that shed into the faeces, ready to infect other animals, these cat and dog hosts are termed definitive hosts. Definitive hosts are the
hosts that the organism was intended for and that the organism reaches sexual maturity in.
In the case of Sarcocystis, Hammondia and Besnoitia, the cat or dog can only be infected by the parasite if it eats the meat or offal of an intermediate host
(usually a herbivore or omnivore) that contains immature forms of this organism encysted in its tissues. This is termed an indirect life cycle: greater than one host species is required by these
organisms. In the case of Isospora, the coccidian organism is able to cycle through the dog or cat population without any need for an intermediate host. Basically, dogs or cats can become infected directly through the ingestion of feces or faeces-contaminated grass and soil containing infectious Isospora parasite cysts. This is termed a direct life cycle:
it is a definite-host to definitive-host lifecycle. It is for this reason that the main species of coccidial organism seen in kittens and puppies is Isospora.
Its lifecycle is far more simple and direct: it can simply be caught from
eating the feces of other cats and dogs - it does not require the animal to predate on
other animals (kittens and pups are too young to hunt).
The final important thing to note is that
cats and dogs have their own coccidia species that only infects them. Cat
coccidia do not infect the intestines of dogs or any other animals and vice versa.
The cat (and dog?) as an intermediate host:
Sarcocystis neurona is a parasite of opossums (opossums are the definitive hosts
that shed infectious Sarcocystis oocysts into their faeces) that can infect a
number of intermediate hosts, including the domestic cat and horse. When oocysts are ingested by a cat, the immature
forms of the Sarcocystis organism replicate within and encyst within the brain
and muscles of the cat. This causes brain disease and severe (often fatal) neurological signs in infected cats - see section 4f for details. Another species of Sarcocystis, dubbed S. canis, may cause liver, brain and skin disease symptoms in dogs. Its
lifecycle is currently unknown.
2b) Livestock animals and coccidia:
Livestock as definitive hosts:
Various species of coccidia are known to cause severe weight loss, ill thrift and intestinal upsets in young livestock animals, particularly animals which are overcrowded and stressed and subjected to physiological stresses
(e.g. excessive growth-rates, frequent pregnancy and lactation, weaning) and poor standards of
hygiene and sanitation. Most species of livestock animal (horses, deer, rabbits, cattle, pigs, poultry, goats and sheep) have their own specific species of intestinal coccidia: Eimeria species tend to be the main species implicated in livestock infections, but Isospora has also been implicated as an intestinal pathogen in pigs.
Pigs, cattle and chickens (and other poultry) raised in intensive farming
situations, are particularly subject to a large variety of stressors (e.g. transportation, malnutrition, other parasites) and environmental conditions facilitating the spread of coccidiosis and, as a consequence of this, coccidia are a major parasitic nuisance affecting these farming systems. Clinical signs (watery to mucoid or bloody diarrhoea, tenesmus, dehydration, weight loss, even death) are similar to those seen in the cat and dog. Millions are spent every year
controlling coccidia in pig, cattle, goat and poultry operations and tonnes of the antibiotic
medications used to control the parasites are put into the feed of such animals, trying to prevent them
from becoming sick and losing weight. This has, naturally, lead to public concerns about the development
of antibiotic resistant bacteria in farming operations (through antibiotic overuse)
and concerns about potentially-toxic antibiotics entering the human food chain.
Some terminology and parasite pointers:
Because these coccidial species (Eimeria, Isospora suis) are able to replicate within the intestines of
livestock animals, achieve sexual maturity in these hosts and create infectious oocysts that shed into the faeces, ready to infect other animals, these livestock hosts are termed definitive hosts. They are the hosts that the organism was intended for and that the organism reaches sexual maturity in. These intestinal coccidia species (Eimeria, Isospora) are able to cycle through the livestock population without any need for an intermediate host: i.e. cattle can become infected directly through the ingestion of
cattle feces or cattle-faeces-contaminated grass and soil containing infectious parasite cysts.
This is termed a direct lifecycle. The final important thing to note is that
each livestock animal species has its own coccidia species that only infects it
(i.e. each species of coccidian is host-specific). Pig coccidians do not infect the intestines of cattle or any other animals; cattle coccidia only infect cattle
and turkey coccidia only infect turkeys and so on. Even sheep and goats differ enough
from each other that goat coccidia do not infest sheep and vice versa.
Livestock as intermediate hosts:
In addition to intestinal coccidiosis, livestock animals may also become infected with
coccidial species that typically replicate and achieve sexual maturity within the intestines of
other, carnivorous, non-livestock animals, including dogs and cats. When livestock
ingest grass that has been contaminated with the coccidia-infected faeces of cats or dogs (and other carnivores), these parasites can hatch out in the livestock animal's intestines and migrate through the
wall of the intestines into the animal's visceral organs (e.g. abdominal lymph nodes, walls of the
blood vessels, liver, muscles and brain). The invading organisms replicate within
and damage the cells of these internal organs until the livestock animal's immune
system responds and suppresses this replication, forcing the organisms to hide out in walled off cysts
with those tissues. These organisms remain living and can lie dormant, hidden within the animal's organs and muscles, for many years. Symptoms of this intermediate host infection may not be observed unless the parasite is a particularly aggressive species (e.g. Sarcocystis tenella in sheep, S. cruzi in cattle); the parasite
damages a vital region of the host's body (e.g. a major blood vessel, the brain)
or the livestock animal's immune system response is particularly weak and the parasite is permitted to run rife and uncontrolled through the organs, creating extensive damage. If the meat (muscle)
or offal (internal organs) of an infected livestock animal is later fed, uncooked, to the
correct carnivore definitive host species, the livestock tissue cysts will reactivate,
hatch out in that carnivore's gut and replicate in the intestines of that animal, thereby causing intestinal infection (+/- clinical symptoms of disease).
Some terminology and parasite pointers:
In this aforementioned situation, the cattle or livestock animal is termed an
intermediate host because the parasite needs this livestock host as part of its lifecycle, but is unable to attain sexual maturity in this host. The carnivore (dog or cat etc.)
is the definitive host in this situation because the coccidia are able to replicate within the intestines of this animal, achieve sexual maturity in this animal and create infectious cysts that are shed in the faeces.
The final important thing to note is that many species of coccidian parasite are specific to only one type of intermediate host animal (e.g. Sarcocystis. tenella
on infects sheep and S. suihominis only infects pigs) and one or sometimes
a couple of definitive hosts within the same carnivore family (e.g. S. tenella
only infects canids, S. suihominis only infects primates). Consequently, if an intermediate host animal consumes a fecally-shed coccidian oocyst that it is not adapted to (e.g. if a pig ate an S. tenella cyst, intended for a sheep) or a definitive host carnivore consumes meat containing a parasitic tissue cyst that it is not adapted to (e.g. if a primate ate sheep meat containing S.
tenella), nothing will happen. The cysts will travel right through the intestines and out into the faeces and cause no issues at all. Only the right definitive host and intermediate
host species can take part in the coccidian lifecycle of each coccidian species.
2c) Wildlife animals and coccidia:
Wildlife - definitive hosts:
A massive range of wild animal species including: Australian macropods (e.g. kangaroos, wallabies), rabbits, hares, opossums, wild livestock species (deer, cattle etc.), frogs, platypus, echidnas, seals, wombats and wild bird species (e.g. birds of prey, pheasants, wild ducks, geese and poultry-types), have their own species of coccidia which replicate within their intestines, sometimes
producing signs of intestinal disease. As occurs with the other, aforementioned, domestic and livestock animal species, the coccidial species affecting wild animals are very host specific: they will only replicate and cause disease in a specific wild animal definitive host species.
 Disease symptoms, when they occur, tend to occur most frequently in young animals, particularly those that are under conditions of high stress, are malnourished
or are infected with other diseases (e.g. other intestinal parasites) or subjected to poor environmental
conditions. For example, coccidiosis is very common in baby, hand-raised marsupials (e.g.
baby wallabies, possums and kangaroos) because they are suffering from the severe stresses of altered diet (sometimes even an inappropriate diet), human handling and loss of their mother.
Severe clinical infestations are also commonly encountered when the juvenile animal first starts to graze pasture (e.g. around 10 months of age in wombats): it is thought that these animals are being exposed to large amounts of coccidia in the pasture, but have not yet developed good enough anti-coccidial intestinal immunity to deal with it. Consequently, the organisms are permitted to replicate freely and these animals develop symptoms of disease. Some wild animal species (e.g. frogs) seem to suffer very little from their enteric coccidial infections, rarely showing any symptoms of disease, whereas other species
(seals, marsupials, echidnas) may often develop severe disease, even death. For example, echidnas often die from a form of coccidiosis that disseminates from their intestines throughout their
internal organs.
Disease symptoms, when they occur, tend to occur most frequently in young animals, particularly those that are under conditions of high stress, are malnourished
or are infected with other diseases (e.g. other intestinal parasites) or subjected to poor environmental
conditions. For example, coccidiosis is very common in baby, hand-raised marsupials (e.g.
baby wallabies, possums and kangaroos) because they are suffering from the severe stresses of altered diet (sometimes even an inappropriate diet), human handling and loss of their mother.
Severe clinical infestations are also commonly encountered when the juvenile animal first starts to graze pasture (e.g. around 10 months of age in wombats): it is thought that these animals are being exposed to large amounts of coccidia in the pasture, but have not yet developed good enough anti-coccidial intestinal immunity to deal with it. Consequently, the organisms are permitted to replicate freely and these animals develop symptoms of disease. Some wild animal species (e.g. frogs) seem to suffer very little from their enteric coccidial infections, rarely showing any symptoms of disease, whereas other species
(seals, marsupials, echidnas) may often develop severe disease, even death. For example, echidnas often die from a form of coccidiosis that disseminates from their intestines throughout their
internal organs.
Wildlife - intermediate hosts:
Similar to the situation described in the livestock section, many species of wild animals (particularly
herbivores and omnivores) are intermediate hosts for a range of carnivore coccidial species. As occurs with the livestock coccidian types, these wildlife coccidia are very host-specific, only encysting and going dormant within the muscles and organs of the correct wild animal species. The coccidian parasite only completes its lifecycle when the intermediate host wild animal is consumed by the correct carnivorous animal adapted to play definitive host to that coccidial organism. Often this definitive host animal is a wild carnivore (fox, wolf, wild cat, dingo, coyote) found in the same environment as the wild intermediate host and the lifecycle takes place completely within the wild (sylvatic) environment, without any involvement from people, their carnivorous
pets or their livestock.
2d) People and coccidia - is the disease zoonotic (infectious to man)?:
Most of the enteric canine and feline coccidian species discussed on this page are not directly or
indirectly transmissible to humans. People should not be worried about contracting
Isospora, Hammondia, Sarcocystis or Besnoitia from their pets.
Humans do have their own specifically-adapted species of coccidian organisms that
can infest them and cause disease within them, however, these tend to come from
interactions with other infected humans, not from interactions with infected pets. Certain species
of intestinal coccidia (e.g. Sarcocystis suihominis, S. hominis) can infest man through the consumption of raw or severely under cooked pork and beef products.
Closely-related protozoan organisms such as Toxoplasma gondii and Cryptosporidium
parvum are capable of infecting people (zoonoses). Sometimes, these infectious organisms
may cause severe disease symptoms and even death in infected humans. People may contract
these organisms from domestic pets and from the consumption of certain under cooked meat products.
These zoonotic organisms will not be discussed further on this particular page, but will
have their own specifically dedicated pages in the near future.

3. Coccidia transmission: how do dogs and cats contract coccidia?
From here on in, we shall leave the livestock and wildlife animals behind and focus
our discussion on coccidia and coccidiosis in the dog and cat. This section contains information
about coccidia transmission in dogs and cats and the role that environmental and host-related
factors play in contributing to and exacerbating the symptoms of disease.
3a) Coccidia transmission in Dogs and Cats.
 A number of species of Isospora are known to infect our domestic pets, in particular:
Isospora felis and Isospora rivolta in the cat and Isospora canis, I. neorivolta, I. ohioensis and I. burrowsi in the dog. This parasite species (Isospora) has no intermediate host requirement and is able to spread from cat to cat and dog to
dog via direct fecal-oral transmission. It is highly contagious. Kittens and puppies (and older animals)
become infected if they consume Isospora-contaminated feces from other cats or dogs and may even reinfect themselves through the consumption of their own Isospora-infected droppings. This is one reason
why owners should not let their dogs and cats consume the stools of other animals.
It is also a reason why dog and cat food and water bowls should not be placed in a position
whereby the food and water could become contaminated with fecal material (e.g. pets stepping into food and water dishes with their poop-covered feet) and, subsequently, consumed.
A number of species of Isospora are known to infect our domestic pets, in particular:
Isospora felis and Isospora rivolta in the cat and Isospora canis, I. neorivolta, I. ohioensis and I. burrowsi in the dog. This parasite species (Isospora) has no intermediate host requirement and is able to spread from cat to cat and dog to
dog via direct fecal-oral transmission. It is highly contagious. Kittens and puppies (and older animals)
become infected if they consume Isospora-contaminated feces from other cats or dogs and may even reinfect themselves through the consumption of their own Isospora-infected droppings. This is one reason
why owners should not let their dogs and cats consume the stools of other animals.
It is also a reason why dog and cat food and water bowls should not be placed in a position
whereby the food and water could become contaminated with fecal material (e.g. pets stepping into food and water dishes with their poop-covered feet) and, subsequently, consumed.
An important thing to note is that the Isospora oocysts shed into a pet's feces are not immediately infective to other animals: they need to mature slightly and develop into an infective form before they can infect another dog or cat. This maturation process
takes at least 8 hours (minimum), which is important to know
because much control of the disease can be achieved simply by cleaning out feces
regularly (two to three times daily), prior to the maturation of the cysts.
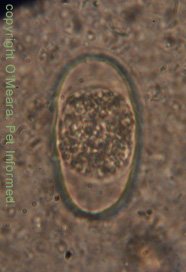
See the image on the right: This is an Isospora canis oocyst from a dog with coccidiosis. The
central ball of cells within the oocyst is in the process of dividing. This fecal sample was only 30 minutes old and the cysts were already starting to divide and mature towards an infective state.
 The main species of enteric Coccidia infecting kittens and puppies is Isospora:
Another thing to be aware of, when it comes to Isospora-infected faeces, is that faeces
infected with this organism do not have to look abnormal and nor do they have
to come from a kitten or puppy. Isospora is not only found
in obviously-diseased, slimy, bloody-looking diarrhoea specimens (e.g. the image on the right). The organism can be found in perfectly formed, normal-looking faeces produced by subclinically infected kittens,
puppies and adult animals. Coccidia carriers (animals that have the infection and are shedding
the organisms in their faeces, but which show absolutely no symptoms of disease) are very common
in the dog and cat population and their faeces, though normal-looking, can be highly infective to other, more-susceptible animals.
The main species of enteric Coccidia infecting kittens and puppies is Isospora:
Another thing to be aware of, when it comes to Isospora-infected faeces, is that faeces
infected with this organism do not have to look abnormal and nor do they have
to come from a kitten or puppy. Isospora is not only found
in obviously-diseased, slimy, bloody-looking diarrhoea specimens (e.g. the image on the right). The organism can be found in perfectly formed, normal-looking faeces produced by subclinically infected kittens,
puppies and adult animals. Coccidia carriers (animals that have the infection and are shedding
the organisms in their faeces, but which show absolutely no symptoms of disease) are very common
in the dog and cat population and their faeces, though normal-looking, can be highly infective to other, more-susceptible animals.
The infective cysts of Isospora are somewhat resistant to the effects of sunlight, desiccation, freezing and numerous disinfectants and they can persist in the environment
and in dog and cat facilities for a very long period of time (many months), long after the visible feces
themselves have broken down and disappeared. Consequently, wherever there has been coccidia-contaminated
feces in the past (indoors or outdoors), there are potentially infectious coccidia organisms still remaining
in the environment. Just because you can't see any droppings does not
mean that the surfaces: pavement, concrete, dirt/soil, lawn, cages, food bowls, grooming equipment, ground or vegetation are not infective to your dog or cat. The puppy that you have just taken to the park could walk across contaminated ground and come home, lick its feet, and get infected
by parasitic oocysts in microscopic faeces that you didn't even see!
Dogs and cats can also ingest infectious particles when they lick the shoes, hands or clothes
of a human that has been in hands-on contact with an affected animal. Those hands and clothes may look clean and may have even been washed, but infectious coccidia cysts might still be
alive on them. Cats and dogs which bite and lick the fur of infected animals may also contract
the organism. Animals spread protozoan cysts onto their fur through rolling in or lying in feces or through licking their feces and then licking their bodies (the cysts are transferred
from the tongue of the animals onto the coat).
In addition to direct fecal-oral transmission (the direct lifecycle), it is also possible for Isospora to
establish an intermediate host life-cycle (termed an indirect lifecycle). Infective Isospora cysts, shed in the feces
of infected dogs or cats, can be consumed by a range of mammalian intermediate hosts, including
various rodent species (i.e. perfect prey animals for the cat or dog), when they eat grain
or grass that has become contaminated with dog or cat feces. Once consumed, these Isospora parasites hatch out in the rodent's (or other animal's) intestines and migrate through the wall of the intestines to the rodent's visceral organs (abdominal lymph nodes, lungs, liver, muscles, brain etc.). The invading Isospora organisms do not replicate within the cells of these internal organs like other coccidial species do. They just
hide out singularly in walled-off cysts within the tissues - here they can lie dormant, hidden within the animal's organs, for many months. Because the organisms do not replicate
within the rodent, symptoms of the infection in the rodent intermediate host will generally not be observed. If the meat (muscle) or offal (internal organs) of the infected rodent is later consumed by a predatory cat or dog, then (provided that the predatory carnivore is the correct definitive host species for the particular coccidial cyst species) the walled-off cysts will reactivate and hatch in that carnivore's gut.
The reactivated organisms will replicate in the small intestine and colon of the dog or cat, thereby causing intestinal infection (+/- symptoms of disease).
In the case of the Hammondia, Besnoitia and Sarcocystis species which infect the dog or
cat intestine, there is no direct, fecal-oral life-cycle. These organisms can only be contracted by a dog or cat through the consumption of uncooked meat or organs from an infected
intermediate host. Depending on the coccidial species involved, intermediate host
animals include: rodents (esp rats and mice), rabbits, camels, cattle, sheep, pigs, buffalo, deer, goats, horses,
poultry and, potentially, many species of wild herbivores and omnivores (e.g. marsupials). Basically, any kind of uncooked meat or offal could harbor infectious parasites
that might infect your dog or cat, should you choose to feed your pet these foodstuffs.
3b) Environmental and host factors that contribute to coccidia transmission in dogs and cats.
Given that Isospora (the main coccidia type commonly found in puppies and kittens)
is most commonly transmitted through the direct consumption of infected feces and via faecal contamination of food and water bowls and the general environment (e.g. grass, soil,
cages, runs etc.), it follows that most dog to dog or cat to cat infections will occur when large numbers of cats or dogs are placed in enclosed conditions, in very close proximity to each other. The larger the number of animals in the one area, the more
likely it is that at least one or more of these animals will be shedding infectious particles
into their faeces, which can subsequently infect the others. Direct fecal-oral contact
is particularly likely if animals are all placed in the one enclosure together
(often litters of kittens or puppies will be placed in the one cage or run together,
not in individual cages, thereby promoting the spread of coccidia among them) or if
fecal run-off from one cage or enclosure is permitted to leak over into adjoining
runs and cages, thereby carrying infectious disease particles to a whole new group of
animals.
Compared to the direct, fecal-oral, route of coccidial transmission, described above, the role that predation and the consumption of intermediate host tissues plays in the transmission and manifestation of the disease is much less significant. Given that very young animals
are the ones most likely to show clinical symptoms of disease but the least likely to hunt for prey, it is unlikely that very young kittens and puppies are going to contract symptomatic coccidiosis as a result
of their own hunting activities. The most likely source of intermediate host infection for these young, susceptible animals would come as a result of a bitch or queen regurgitating raw meat, offal or prey tissues to her litter. The consumption of intermediate host tissues and
consequent infestation with coccidian organisms is much more likely to occur in older
animals (cats and dogs that regularly hunt or fossick for carrion, hunting dogs fed on the offal and meat of their kills, adult dogs fed a bones and raw food and meat diet (BARF diet) and stray or feral animals forced to hunt for their own survival), however, given the role that age, immunity and stress plays in the manifestation of disease symptoms (see following points), it is unlikely that many of these infected
adult animals will actually go on to display symptoms of disease (unless there is something very wrong with their immunity). Additionally, since many of these
coccidian species (Isospora excluded) actually require an intermediate host as an obligatory (essential) part of their lifecycle, this sub-clinical infestation of the adult animal is unlikely to pose a risk to the young and susceptible animals
the adult animal associates with.
Author's note: Isospora could potentially enter a facility through the consumption
of undercooked meat or predated-upon rodents by an adult animal. The parasite could then
spread rampantly through the entire facility because of the direct fecal-oral lifecycle
that Isospora is capable of. Unlike the other species mentioned, Isospora is
not reliant on intermediate hosts to complete the lifecycle and spread the infection.
Whether or not an animal infected with Isospora or any of the other coccidian
parasites actually goes on to develop symptoms of disease largely depends on the integrity of the animal's immune system, the health of its intestinal tract and the number and virulence of the organisms ingested. From an animal husbandry viewpoint, conditions with high fecal contamination levels; poor sanitation; moderate to high humidity levels
(moist air); warm temperature levels and conditions where animals are frequently exposed to
extremes of cold, heat, humidity (excessively wet or dry air) and draughts; poor nutrition or changes in nutrition; animal overcrowding; physiological stressors (lactation, pregnancy, weaning, growing); other diseases; excessive exercise fatigue and transportation all predispose to
coccidia manifestation and spread.
High fecal contamination levels and poor sanitation:
High levels of fecal contamination in an animal's environment obviously facilitate the spread of any fecally-transmitted diseases. In the case of coccidiosis, the chance
of a susceptible animal contracting the organisms increases with the amount of time that the faeces are left lying
around: the longer the faeces remain in the environment, the more oocysts are able to
mature and reach their infective stages. High levels of faecal contamination also play
a significant role in the manifestation of coccidia symptoms because, one, poor sanitary conditions
cause stress to the animals that must endure it (stress suppresses the immune system's
defenses) and, two, poor sanitary conditions promote the spread of other intestinal diseases
including bacterial infections and other enteric parasites (e.g. worms). These other
infections damage the intestinal wall, making the intestine less able to resist the effects of
the invading coccidia, and, two, these additional infections take up some of the attention of the animal's immune system defenses, diverting them
away from fighting the invading coccidia (thus signs are more likely to be seen).
Poor nutrition:
Poor nutrition (which includes both malnutrition and incorrectly-balanced nutrition),
has a huge role in the manifestation of coccidial disease symptoms. Good
nutrition is vital to intestinal health and maintaining the integrity of the lining of
the intestinal tract. Poor nutrition leads to a breakdown in the alimentary tract's
structure and alters the intestine's defenses and motility, thereby making it less able to resist the effects of the invading coccidia. Poor nutrition also results
in a weaker immune system that is less able to fight coccidial diseases: immune cells require
good nutrition in which to multiply and function. Animals that are starving are more
likely to try to hunt for themselves, leading to the increased consumption of intermediate hosts
and encysted coccidia. Additionally, animals that are starving or that are deficient
in certain nutrients are more likely to ingest grass, vegetation, soil and even the
feces of other animals, leading to the increased uptake and consumption of coccidial
organisms (the more organisms ingested, the greater the chances of that animal showing clinical
signs of disease).
High air humidity levels and warm temperatures:
High air and ground humidity levels increase the risks of coccidial transmission because these organisms
tend to survive longer (hang around longer) in wet, humid environments. Temperature
also plays an important role: coccidial oocysts tend to mature to their infectious stages
fastest in environmental temperatures ranging between 20-37 degrees Celsius (Greene CE).
The faster the oocysts mature and become infective, the more likely it is that large numbers of infectious coccidial organisms will be ingested by susceptible animals (the more organisms ingested, the greater the chances of that animal showing clinical signs of disease).
Overcrowding of animals:
Overcrowding promotes the rapid spread of any infectious disease from animal to animal
because there is a much greater likelihood of susceptible animals being placed into close
proximity with infected, pathogen-shedding animals. In the case of coccidia, overcrowding
is of particular concern when lots of stressed kittens or puppies
from all different backgrounds (some infected, some susceptible) are put into runs or cages
together or when older animals (possibly sub-clinically carrying and shedding organisms)
are put into runs or cages with young, susceptible animals (the older ones infect the younger ones). Overcrowding promotes stress, which suppresses the immune system responses of susceptible animals, and overcrowding makes it difficult for facility operators to identify the sick animals and to find a place, sufficiently out of the way, to isolate the sick once they have been identified.
Stressors:
Conditions of extreme or frequently fluctuating heat and humidity, as well as overcrowded conditions; unsanitary conditions; draughty conditions; changes in environment;
transportation; exercise fatigue; weaning; pregnancy; lactation; the presence of other diseases (e.g. parasites and other illnesses) and conditions of inadequate or ever-changing nutrition all contribute
to coccidiosis manifestation and spread. This is because all of these conditions result in high levels of animal stress: stressed animals have poorer immune systems and, as a result of this, are more likely to show signs of infection.
Even adult animals, when placed under enough stress, can develop enough immune suppression
to display clinical signs of coccidiosis (disease symptoms normally affecting the young).
Stressed animals, in addition to being more likely to show signs of disease, are also
more likely to shed larger numbers of infectious cysts into their immediate environment
(the lack of immune system defenses allows the organisms to breed freely and produce
greater numbers of infectious oocysts). High levels of oocyst shedding pose a much greater risk of infection to other susceptible animals.
Immune suppression:
Aside from stress, there are many other causes of immune suppression that can affect young or adult animals. These include genetic immune system disorders (seen from a
young age) and acquired immune system depression (e.g. immune mediated diseases, immune
suppressant drugs, chemotherapy, cancer, diabetes mellitus, Cushing's disease, infectious immunosuppressant diseases, bone marrow disorders). Individual animals afflicted with these disorders are more likely to
show clinical signs of coccidiosis and more likely to shed large numbers of infective coccidial oocysts into their faeces.
3c) Real-life situations that promote dog to dog and cat to cat transmission of coccidia:
Obviously, some environments are more risky for coccidial infection and transmission than others. Environments that are likely to have had coccidia in the past (and are thus at higher risk of still containing the infectious particles) include pet shops, shelters, breeding facilities, 'puppy farms' (backyard breeders), pounds, grooming facilities, dog clubs and, ahem, veterinary clinics.
1) Boarding kennels and catteries:
Kennels and catteries often house large numbers of dogs and cats in close proximity; these animals are often stressed (which lowers their immunity to disease) and the facilities are often designed to be of a more enclosed, space-conserving, compact structure, rather than an open-planned, spacious structure. There is a much greater chance of fecal material and infectious disease particles spreading between cages that
are closely-aligned, both through direct animal contact (face-licking etc.) and fecal run-off.
The one thing in their favor is that boarding kennels and catteries do not often board extremely young animals, thereby removing the most susceptible individuals from consideration.
2) Pounds and shelters:
This is probably the worst situation for coccidia transmission. Susceptible animals are often
kept in overcrowded conditions, in very close proximity to each other; puppies and kittens
of different backgrounds are often placed in cages together because of insufficient space; conditions are often unsanitary (depending on the shelter or pound in question); animals are often very stressed and of poor nutritional status (this lowers their immunity to disease) and their vaccination and worming history is generally very poor (the animals may have other
intestinal viruses and parasites, increasing their susceptibility to coccidial disease). In addition to this, young puppies and kittens (the most susceptible animals) make up a huge proportion of shelter and pound accessions - litters of unwanted pups and kittens are dumped at such facilities by irresponsible
owners every week of the year.
3) Pet Shops:
As far as coccidia transmission goes, pet shops often do not rate that much above pounds and
shelters. Pet shops often keep very young puppies and kittens in overcrowded conditions, in very close proximity to each other; puppies and kittens from different backgrounds are often placed in cages together (increasing disease spread between 'clean' and susceptible animals); conditions are sometimes unsanitary (depending on the pet shop in question) and animals are often very stressed and of poor nutritional,
vaccinational and worming status. Sadly, many pet shop pups and kittens are poorer quality animals that have been offloaded by backyard breeders or irresponsible pet-owners
who have 'ended up with a litter' - this makes their quality, immune status and background
(including worming and vaccination status) an unknown factor. In addition to this, young puppies and kittens (the most susceptible animals) make up the vast majority of pet shop sales (those
cute faces and fluffy bodies make for an ideal 'impulse buy').
4) Breeding facilities:
Vaccination, worming and parasite control tends to be adequate among most breeding populations. Coccidia, if it does manage to get into a breeding colony, is likely to spread rapidly throughout the breeding facility, however, because of the number of animals located in close proximity to each other; the number of underage, highly-susceptible
animals around (newborn puppies and kittens etc.) and the high levels of stress that can occur
in bitches and queens who are pregnant and lactating and in pups and kittens that are being weaned.
3d) My pet hasn't been near another dog or cat in months - how could he or she get coccidia?
Having read up to this point, the numerous reasons for this should now be pretty self-explanatory, however, I will group those reasons together in this section for completeness. The following
points describe ways in which clinical signs of coccidia infection may occur in pet animals
that have not been near another cat or dog in months.
1) Reactivation of coccidia in a carrier patient:
Coccidia are able to replicate within the intestinal tracts of all dogs and cats
(young or adult), however, they only tend to create symptoms of disease in very young animals. It is not uncommon for animals that have been infected (older cats and dogs or young animals which have recovered
from a clinical bout of the disease) to develop a 'harmonious' and balanced co-existence
with the coccidian parasites infesting their intestines (a situation termed premunition).
These animals have generally developed enough immune resistance to the organisms that the
organisms do not cause symptoms of disease in them, but not enough immune resistance that they are
able to completely clear the organisms from their intestines. These animals (termed
carriers) can shed coccidia in their faeces for long periods of time (months to years),
showing no symptoms of disease because organism and host are in harmony. If, however, the host suffers from any form of immune suppression (including stress-induced immune suppression) or intestinal dysfunction (e.g. ulcerative intestinal diseases, other parasites, bacterial infections), this delicate balance of host and parasite can be broken. The coccidia will reactivate and breed profusely
within the host animal's intestines, creating symptoms of disease in an animal that might not have
seen another dog or cat for months.
Interestingly, most antibiotics and coccidiostats used in coccidia therapy do not
destroy all of the coccidial organisms. Most of them simply kill enough of the organisms
that they won't decimate the bowel, thereby buying time for the immune system response to
kick in and establish this state of host-parasite balance and neutrality. Animals
treated in this way will 'seem' to have recovered from the disease, but more often than not, they will simply have converted to a non-clinical carrier state. Consequently, if these hosts then go on
to develop any form of immune suppression or intestinal dysfunction, there is every likelihood
that this delicate balance will be broken. Again, the coccidia will reactivate and breed profusely
within the host's intestines, creating symptoms of disease in an animal that might not have
seen another dog or cat for months. When this occurs, pet owners will often blame the
vet for giving the wrong antibiotics to their pet (or not treating the correct disease), when the
real problem is the underlying nature of the coccidial organism (its tendency to persist despite treatment)
and the presence of some underlying stress or disease factor that keeps upsetting
the balance.
2) Coccidia persistence in the environment:
As mentioned previously, coccidian parasites are quite resistant to environmental
conditions such as desiccation, heat and cold and are able to persist in the environment
and on clothing and fomites (dog dishes and water bowls) for long periods of time. Your animal can contract the highly contagious organisms from ingesting infected feces, soil and vegetation and from licking fecally-contaminated clothing and fomites without ever going near another dog or cat. Contracting the disease can be as simple as eating poo in the park.
3) Ingestion of intermediate hosts:
Certain species of coccidia, including the highly-contagious Isospora organisms, are
able to be transmitted to dogs and cats following the ingestion of the uncooked meat (muscles)
and offal (organs) of infected intermediate hosts: various livestock, rodent and
wild animal reservoirs. Dogs and cats can consume these tissues as a result of their own
hunting activities (e.g. cats can catch coccidia through their mousing activities) and foraging
activities (roaming dogs may eat rotting carcasses) or they may be fed these tissues
by owners who are unaware of the potential for raw-meat disease transmission (e.g.
hunters who feed their pets raw offal, pet owners who subscribe to a 'natural' raw meat
and offal diet). These dogs and cats do not need to meet another dog or cat in order to
contract the disease.
Interestingly, in the case of Isospora, the animal can contract the organism from
eating coccidial cysts in raw meat and offal meals, but then go on to reinfest itself
over and over through the consumption of its own infected fecal materials (fecal-oral route). This can result in dogs or cats developing significant coccidial parasite burdens
without ever seeing another dog or cat.

4. Symptoms of coccidiosis in dogs and cats - what does coccidia do to your pet?
As mentioned in the opening sentences, coccidiosis is a disease caused by certain species of microscopic protozoan parasites that is characterized by small intestinal and (sometimes) colonic disease symptoms, including: watery to mucoid (custard-consistency) diarrhoea, fresh blood in the stools, straining to defecate (tenesmus), flatulence, dehydration, blood loss (anemia), weight loss, weakness and, sometimes, abdominal pain and vomiting. The following discussion is mostly for those of you who are interested in how these protozoan parasites infect the gastrointestinal tract of the dog and cat and create the coccidiosis symptoms observed. Understanding how the infectious disease organisms work is useful because it aids your understanding of why the various symptoms occur; what complications can develop; how the disease is spread and what treatments are available.
This section will only focus on the replication of coccidia species within the small intestine and colon of the dog and cat. These animals are, after all, the main animals that actually present to small animal veterinary clinics with symptoms attributable to coccidial infection. Aside from Sarcocystis neurona (see section 4f), which does infest intermediate host felines as part of an indirect lifecycle, coccidia infections in intermediate host animals shall not be discussed further. In the case of coccidial infections (Eimeria etc.) that do infest the intestines of wild and livestock animal definitive hosts, for ease of
simplicity, these definitive host wild animal and livestock infestations can be thought of as being similar to that which occurs in our pet dogs and cats.
4a) How coccidian parasites cause disease (how they replicate within and destroy cells).
1. The coccidia stages infective to the dog and cat - what they are and how they form:
The stages of a coccidian organism that are infectious to a dog or cat definitive host are those that are present within an oocyst or that are encysted within the muscles or organ
cells of an intermediate host.
Infectious oocysts - what they are and how they become infectious:
An oocyst is the highly infectious,
environmentally resistant form of a coccidian parasite that is shed into the feces of
a definitive host and which can be subsequently ingested either by a similar species
of definitive host (direct lifecycle as seen with Isospora) or a different species
of animal: an intermediate host (indirect lifecycle as seen with Isospora, Hammondia, Besnoitia and
Sarcocystis). Before an oocyst can become infectious to any other host animal, definitive
or otherwise, it needs to mature. The oocyst undergoes maturation in the environment:
its internal cells divide and differentiate many times (like an embryo), eventually forming several sporocysts
containing several sporozoites. Sporocysts are sub-compartments encased within the
tough, outer shell of the oocyst and sporozoites are independent, living, infectious protozoan organisms, encased inside the sporocyst compartments. The number of sporocysts and sporozoites that form, encased within each oocyst,
varies depending on the species of coccidian: mature, infectious Isospora oocysts
have 2 sporocysts, each containing 4 infectious sporozoites inside them, whereas infectious
Hammondia oocysts contain 8 sporozoites with no sporocysts (compartments) to contain them.
Author's note: Sarcocystis matures inside the definitive host's intestines. It is mature and infective
as soon as it exits the host in the droppings.
Infectious tissue cysts in the intermediate host - how they form:
When a mature, infectious oocyst is eaten by an intermediate host animal, the tough shell of the
oocyst breaks down in the animal's intestines, along with the internal compartments (the sporocysts). This allows
the infectious sporozoite organisms to break free. The individual protozoan
sporozoites (each free-living and migrating independently of the other sporozoites) migrate through the wall of the intermediate host's intestines, travel throughout the animal's body and invade the cells of various organs and muscles (the liver cells, muscle cells, blood vessel cells and brain cells
of the intermediate host are favored). When a sporozoite invades an animal cell, it multiplies rapidly within that cell by undergoing asexual reproduction (simple cell division). Hundreds of parasite protozoan clones are produced as a result of this asexual replication, all clustered together inside the single animal cell. When viewed under a microscope, they look like a ball of banana-shaped organisms all gathered within a cell. The individual, rapidly-dividing protozoans, within this cluster of organisms, are now termed tachyzoites instead of sporozoites (they are individual protozoans that replicate fast - tachy means fast). When the multiplying tachyzoite organisms inside the cell become too numerous, the host animal cell will rupture and die, releasing all of the organisms into the surrounding
tissues. The individual, free-living protozoan organisms (still termed tachyzoites or, alternatively, merozoites), swim away independently, invading more cells and replicating rapidly inside those cells (forming more tachyzoite organism clusters) and continuing the cycle of infection and protozoan replication.
This rapid cycle of organism replication and cell-death is only stopped when one of two things happens:
1. The animal's immune system responds to the invasion, killing all the freely-migrating merozoites/tachyzoites it finds. The only way that the protozoan organisms are able to avoid this immune system attack is by hiding out inside of the animal cells in their clustered forms. They alter their activity, only replicating very slowly and only to the point whereby there are many
protozoans in the cluster, but not enough to destroy the protective host cell shielding them.
The replicating organisms don't want to be exposed to the immune system attack that would occur were they to destroy their protective host cell. These slowly dividing protozoans, lying dormant within the cells of the host animal, are now termed bradyzoites (brady means slow). They are essentially the same as the tachyzoites except that they replicate very slowly and go dormant inside of animal cells, (tachyzoites, in contrast, replicate rapidly in cells and aggressively destroy host cells). These bradyzoites may reactivate, increase their activity and resume rapid, tachyzoite-type replication
within the intermediate host's cells if the host's immune system fails.
AND/OR
2. The parasite fulfills its maximum number of tachyzoite (rapid) replications.
Many species of coccidian are programmed to only undergo a fixed number of
rapid (tachyzoite) cell-invasion and asexual replication repetitions, after which they automatically reduce
their activity and revert into the dormant, slow-growing, tissue-encysted bradyzoite forms. These can only reactivate and continue their life cycle after being ingested by a definitive host.
Either way, the end result of this process is the formation of clusters of bradyzoites within the tissue cells of the intermediate host animal. These bradyzoite clusters are the infectious muscle and organ 'cysts' that can infect a dog or cat (definitive host)
when it eats the muscles and organs of an intermediate host. In many coccidian lifecycles, only the dormant or slowly-replicating bradyzoite forms are able to infect dogs and cats, whereas
the similar-looking, but rapidly-dividing, tachyzoite forms are not infectious to these definitive hosts.
2. What happens when a dog or cat eats an infective coccidial stage (how symptoms are created).
When a dog or cat ingests the infectious, mature-stage oocysts of a coccidian organism, or ingests infectious bradyzoite-containing organs or meat of an intermediate host animal, the oocysts or bradyzoite-cysts travel through the gastrointestinal tract to the small intestine
and sometimes the colon. When the parasite cysts/oocysts reach these regions, they 'excyst' (hatch). In the case of ingested oocysts, the rigid outer wall (shell) of the
organism breaks down, along with the internal sporocyst compartments, releasing the infectious
sporozoites into the intestinal fluids. In the case of ingested bradyzoite cysts, the host tissues surrounding the 'ball of organisms' breaks down in the intestinal digestive fluids,
releasing the individual organisms (now termed merozoites instead of bradyzoites) into the digestive fluids.
The infectious organisms (sporozoites from an oocyst or merozoites from a tissue cyst) invade the epithelial cells (the surface layer of cells) lining the walls of the intestines.
They also enter the intestinal cell-layers deep to these - the lamina propria (LP) cells.
When the individual protozoan organisms invade these intestinal-lining cells, they replicate asexually inside of them, similar to the situation that was described in the intermediate host tissues, forming clusters of rapidly-multiplying intracellular protozoans. When these organisms multiplying inside of the intestinal cells become too numerous, the host cells rupture and die, releasing all of the newly-created organisms into the surrounding
tissues and into the intestinal tract. These individual protozoan organisms (termed merozoites), swim away independently, invading more intestinal-lining cells, replicating rapidly inside these cells and continuing the cycle of infection and protozoan replication. This process, whilst it is occurring, causes massive amounts of intestinal cell damage, resulting in the clinical symptoms seen in puppies and kittens with coccidiosis (see section 4b on symptoms).
As mentioned in the intermediate host section, many coccidians are only able to undergo
a fixed number of cell-invasion and asexual replication repetitions. This is true for the replication
situation that occurs within the definitive host's intestinal cells too. In this situation, however, instead of the final-replication merozoites remaining in a dormant, clustered
bradyzoite form (as would occur in the intermediate host), the final-replication
merozoite forms in the intestinal cells of the definitive host set about producing
infectious, fecally-distributed oocysts.
3. How the infectious oocysts are created.
Following the final asexual replication phase, the merozoites produced are released into
the intestines (or local intestinal tissues). Each individual merozoite invades an intestinal
cell but, instead of replicating asexually like it did before, it differentiates (matures) into either a
single, very large, female merozoite (termed a macrogamete) or subdivides itself
into many, much smaller, male merozoites (termed microgametes). These microgametes
have swimming 'tails' termed flagellae (much like human sperm cells do) and, once mature, they
exit their host cell and swim over to other intestinal cells, hunting for mature female
macrogametes. Upon finding one, the male microgamete enters the intestinal cell holding the female protozoan macrogamete and fertilizes that macrogamete. This combining of
male and female gametes is termed sexual reproduction and it results in the formation
of a zygote (a fertilized 'egg'). A rigid wall forms around the fertilised zygote
and, once this wall is firm enough to withstand the harsh world outside of the intestinal
tract, it erupts from the intestinal cell and gets shed into the faeces as an oocyst. Oocysts are shed in large numbers when lots of protozoan replication is occurring
and clinical signs are evident. They are also shed, albeit in much smaller numbers, when a coccidia carrier state develops and no symptoms are seen (see next paragraphs).
From the time of ingestion of the infectious oocysts or intermediate host tissue cysts, it takes 4-11 days
for the first oocysts to appear in the faeces of the definitive host animal (depending on the coccidian
species). This period is termed the prepatent period.
4. Development of a non-clinical coccidial carrier state (the role of the host immune system in the appearance of clinical symptoms):
The cycle of organism replication and intestinal cell-death is only stopped or slowed
when the definitive host animal's immune system responds to the invasion, killing all the freely-migrating merozoites it finds. The only way that the protozoan organisms are able to avoid this immune system attack is by hiding out inside of the animal cells in their clustered forms. These organisms alter their activity
and reproductive processes, only replicating very slowly and only to the point whereby there are many
protozoans in the cluster, but not enough to destroy the protective host cell shielding them.
The replicating merozoites don't want to be exposed to the immune system attack that would occur were they to destroy their protective host cell. These slowly dividing protozoans, lying dormant within the intestinal cells of the definitive host animal, can be
termed bradyzoites (brady means slow).
Author's note: as mentioned in the intermediate host section of section 4a
(tissue cyst section), many coccidians are only able to undergo a fixed number of asexual replication repetitions. When the definitive host's immune system response kicks in, instead of these final-replication-stage merozoites erupting from their intestinal cells and differentiating into their sexual replication forms (ready to produce oocysts), many will choose to remain protected in their intestinal cells in dormant bradyzoite forms. After all, there is no point coming out of the intestinal cells only to be killed by a waiting immune system. These organisms bide their time, waiting for a 'break in the immune system' to occur, whereupon they will reactivate and
come out of the intestinal cells (when it is safe to do so) and continue the process of oocyst formation.
Bradyzoite protozoan organism clusters are not killed by antibiotics because they hide inside of cells where the antibiotics can't reach them, and, despite the fact that these organisms are forced to massively suppress their rapid-growth-rates in response to the immune system's presence, they are not actually killed by the immune system
either. Consequently, in an animal with a healthy immune system, a situation will develop whereby
the animal is infected with intestinal coccidiosis, but, due to its strong immune system defenses, will have very little protozoan organism replication, very little intestinal cell injury
and, consequently, no clinical signs. This is the coccidia carrier state. Some oocysts will still manage to evade the immune system's attack and get produced from time to time, but the numbers will be low compared to the numbers of oocysts produced during clinical infection. These oocysts will infect the environment and sometimes get detected on fecal floatation tests (see section 5 - coccidial diagnostics), but the animal will not show any signs of disease.
If the immune system's defenses start to fail (e.g. through immune suppressant diseases, through immunosuppressant drugs, through stress, concurrent diseases etc.), the bradyzoites in the cells of the intestine will reactivate in the presence of this lax defense system. They will revert to a more aggressive form of asexual and sexual replication: replicating rapidly, causing lots of cell invasion and intestinal cell damage
and creating clinical signs of infection. During this period of reactivation, lots
of gametes will be formed from final-stage merozoites and plenty of infectious coccidial oocysts will appear in the faeces. It is for this reason that animals with long term or repeated bouts of clinical, symptomatic coccidiosis need to be examined for
an underlying immune system or stress-related problem. Normal animals should not keep
getting clinical coccidiosis - their immune systems should be able to hold coccidia in check!
Author's note: One of the short-falls of fecal flotation (see section 5), the major diagnostic test for coccidiosis, is the issue of 'intermittent coccidia shedders'. These are animals
affected with coccidia that only release oocysts into their feces every few days or weeks, thereby making coccidia carriers very difficult to detect on a routine faecal float. It is thought that this intermittent shedding occurs as a result of natural ebbs and flows in the animal's immunity. The immune system regularly and periodically (due to physiological stresses, rhythmic hormone shifts etc.)
releases some of its control over the coccidia for a brief period of time, long enough for some of the
coccidia to reactivate and make and shed oocysts, but not long enough for clinical signs to appear.
4b) Coccidia symptoms (coccidiosis) - the effects on the intestinal tract.
1. The roles of a normal gastrointestinal tract:
The gastrointestinal tract (stomach, small intestine, colon and rectum) of the dog and cat is lined by a thin layer of cells termed an epithelium (i.e. the intestinal and colonic epithelium) or a mucosa. These cells have many important roles including:
1) secretion of mucus: Certain cells of the intestinal tract epithelium (especially the colon)
secrete a protective mucus which is designed to protect the intestinal cells from the abrasive effects of
food and feces passing along the tract and from the erosive effects of bacterial toxins and digestive
enzymes. The mucous also captures infectious organisms (bacteria, viruses and protozoa) that enter the intestinal tract and facilitates their expulsion with the faeces. The mucus
produced also lubricates everything, making the droppings slide along the intestinal tract easily. Intestinal mucus production will increase radically in the presence of intestinal irritants and chemicals, including infectious diseases like coccidiosis.
2) forming a cell barrier: The epithelial cells of the alimentary canal form a physical barrier, preventing bacteria and
viruses and protozoans within the gastrointestinal tract from entering the deeper intestinal
tissues, bloodstream and other organs.
3) gastric motility and expulsion of contaminants: The gastrointestinal tract
is always moving, through the action of powerful muscles located within the walls of the stomach, small intestine and colon. Gastrointestinal motility allows bacterial toxins, invading
organisms and excessive bacterial populations to be removed from the intestinal tract, so that they can
not do as much damage. In the face of invading organisms and toxins, intestinal motility is often increased on purpose in an attempt to expel the invaders from the intestine: this results in diarrhoea. When the intestine is unable to move (is paralyzed), as a result of certain diseases
and drugs, bacterial populations in the bowel can multiply to vast numbers, resulting
in intestinal injury and sickness.
4) colonic motility and absorption of water: The colon has a special role in the absorption
of water from the intestines - this helps to keep the body hydrated. The colon actually uses some of its
motility in a retrograde (backwards) fashion in an attempt to keep faeces inside the colon for just that bit longer so that water absorption can be optimised. Diseases that reduce
segmental colon motility can stop the colon from retaining feces and absorbing the water - watery diarrhea results.
5) transfer of nutrients into the blood: The intestinal tract (especially the small intestine)
is the region of the body where nutrients (fats, proteins, sugars, minerals and vitamins) from the food
are absorbed. Severe intestinal damage and diarrhea (which makes food move through
the tract too quickly for it to be absorbed) can result in malnutrition, weight loss
and mineral and vitamin deficiencies. The cells lining the intestinal tract (the epithelial cells)
have a huge role in nutrient uptake - certain chemical secretions and 'gate-ways'
present on the surfaces of these cells are needed in order for some nutrients to get absorbed.
6) absorption of water: The colon (end of the intestinal tract) absorbs
most of the water that enters the intestinal tract (both through drinking
and through digestive fluid secretions). If the colon is unable to perform this vital
role, severe, life-threatening diarrhoea and dehydration will result.
7) other roles: The intestinal epithelial cells have many other vital roles. They secrete hormones and enzymes which play an essential role in the control of food digestion and intestinal motility. They produce certain digestive enzymes and stomach acids; they initiate nerve impulses that tell the animal when it is full; they secrete hormones that control the intricacies of pancreatic cell and bile duct secretions and they secrete hormones that control the intricacies of intestinal motion.
2. Which coccidia cause intestinal symptoms in dogs and cats?
The pathogenicity of the coccidia (the ability of the coccidian species to cause disease symptoms)
depends on many factors including:
1) the number of oocysts eaten - large numbers of oocysts ingested at any one time can cause rapid-onset, severe disease.
2) how rapidly the organisms divide - the faster the coccidian organisms divide asexually, the quicker the host cells are destroyed and more cells become invaded.
3) the size of the replicating cysts (tachyzoites) - larger cysts release greater numbers of infectious merozoites into the intestine to invade more cells and create more damage.
4) the number of replication cycles needed - coccidia with higher numbers of tachyzoite replication cycles
are able to invade more cells and create more damage before they are forced to become dormant
in their bradyzoite forms or convert into sexual, oocyst-making forms. Coccidia with higher replication cycles may, however, experience a greater delay before the infectious oocysts will appear in the faeces.
5) invasiveness elsewhere - some coccidia species will leave the intestine of the definitive host
and invade and replicate within tissues elsewhere in the host's body. This may result in nasty disease symptoms, similar to those seen in some intermediate hosts. Generally, this phenomenon only occurs in very immune suppressed animals and in certain, specific host
animal species (e.g. echidnas).
Isospora is responsible for most of the intestinal symptoms of coccidiosis seen in the dog and cat.
Hammondia and
Besnoitia do not cause intestinal disease in dogs and cats, despite replicating in their intestines, and require no treatment.
Sarcocystis, likewise, does not cause
intestinal disease symptoms in the dog and cat, however, some species of
Sarcocystis may invade other organs of the dog and cat intermediate host, (e.g. the brain) and produce life-threatening symptoms relative to these areas (see section 4f).
3. The initial stages and symptoms of coccidia infection.
When the cells of the intestinal and colonic epithelium become heavily infected with replicating coccidia
organisms (destructive, space-occupying tachyzoites and bradyzoites), they become damaged and start to degenerate. Ulceration of the lining of the gastrointestinal tract (especially the small
intestine) results, leading to severe irritation and inflammation of the affected regions.
This severe inflammation and irritation of the bowel lining causes the intestines to spasm and the affected animal to display symptoms of abdominal pain. If the colon (large intestine) is also
infected, the animal will display symptoms of colitis - flatulence, straining to defecate
and increased the frequency of defecation. Typically, animals with colitis (inflammation
of the colon) will repeatedly and frequently squat as if needing to do a poo. Owners often think that their pet's repeated posturing and straining to defecate (termed tenesmus) is a sign that their pet has constipation. Animals with coccidia-induced colitis are not constipated, however: they just have a very irritated colon which keeps 'telling
them' that they need to go to the toilet. Some animals will even vocalize (cry, whine) when straining to defecate because of their colon pain - this increases owner suspicions that they are constipated.

 Image 1:
Image 1: A dog with colitis straining to defecate.
Images 2: Blood and mucus-filled faeces, typical of colitis.
In response to the infection and inflammation of the small intestine (and colon),
large volumes of watery, protein-filled inflammatory fluids and mucous flood the intestinal tract. Mucus production, in particular, can be so great that large amounts of jelly-like slime
appear in the droppings and diarrhea of the animal (see the images above). If the amount of inflammatory fluid and mucous entering the intestinal tract is too much for the colon (the major water-absorbing part of the bowel) to reabsorb, then severe,
watery diarrhea will result. This reabsorption of intestinal fluid and mucous secretions
by the colon will be even further impeded in puppies and kittens that develop severe
coccidial colitis in addition to the usual small intestine infestations - inflammation and ulceration of the colon lining results in the colon
not being able to absorb water properly (even the water that these animals drink
may not be absorbed). To add insult to injury, this coccidial diarrhea will often
be further exacerbated by increased intestinal motility: in an attempt to expel intestinal invaders out into the feces, the intestines will deliberately increase
their motility. Unfortunately, this not only pushes out the invading bugs, it also pushes out vast amounts of much needed food and fluid (water), thereby making the reabsorption of water inefficient and the diarrhoea worse. Ultimately, what happens
is that the severe, watery diarrhea and the significant intestinal fluid losses
(the leaking inflammatory fluids and the excessive mucous production) result in an
overall loss of fluids from the animal's body. The young animal can become severely dehydrated
and very sick.
If ulceration of the lower small intestine and colon is significant (i.e. if lots of cells are being destroyed as
a result of coccidiosis), then bleeding can occur. Significant bleeding will become visible
in the stools: it can range from a few small spots or flecks of blood, in amongst
the mucus and slime, right through to large amounts of bright, red blood. Sometimes intestinal bleeding can be so severe that no feces are appreciated - the animal looks as though it is defecating straight blood! This is, as you can imagine, very frightening for owners to see!
Animals with significant coccidiosis and small intestinal damage may display signs of
vomiting, in addition to their diarrhoea. Vomiting further exacerbates the animal's degree
of dehydration because, not only is the animal losing fluid through its liquid stools,
it is also unable to keep any of the water that it drinks down in its intestines.
If ulceration and inflammation of the intestines and colon is significant, affected
animals may also display signs of fever. Symptoms include: a hot mouth and nose, red gums, panting, drinking excessively
and seeking out of cool areas to lie down. The affected animal may also show signs of lethargy and sleepiness during these early stages, both as a result of fever and as a result of
dehydration.
NOTE - fever is not a typical or reliable presentation of animals with coccidiosis (don't rely on it
as a clinical finding).
Author's note: the vast majority of kittens and puppies seen for coccidiosis are not that
severe or sick-looking. They are generally quite bright and alert and playful and they are normally
still eating and drinking very well at home. They may have signs of abdominal pain and they
are often producing vile-smelling, watery to custard-consistency yellow or tan-coloured
droppings containing lots of slime (jelly), with or without the presence of blood. Vomiting
may or may not be seen. These animals often do not need any in-hospital care and they often do fine after some medical treatment at home.
4. Complications of coccidial infection: severe dehydration and protein and electrolyte losses.
If the diarrhoea (+/- vomiting) is severe and is left untreated or inadequately treated, the affected animal can become severely dehydrated. Please remember, dear reader, that these animals will often look as though they are drinking heaps of water. The problem is that
these animals are physically unable to drink enough water to make up for their diarrhoea
losses - much of the water that they do drink will remain unabsorbed and go straight out
the back end! Animals not given appropriate supportive veterinary care (including
intravenous fluid support) can become so dehydrated that they go into shock. Their mouths, feet and ears will become cold to the touch. They will become weak and wobbly on their legs
and may progress to the point of being very non-responsive and unable to walk or lift their heads (cold, floppy puppies and kittens). Their gums will seem pale and dry and cold and their temperatures
may become subnormal (under 37.5 degrees C). Their heart rates will be very fast. Left untreated beyond this point, severe dehydration and shock will cause failure of the liver and kidneys
(organ shutdown) and, eventually, decompensation and slowing of the heart rate (a low heart rate in a
very shocky animal is a very bad prognostic sign) and death.
In addition to dehydration (water-loss), severe inflammation of the gut and the loss of intestinal
secretions through the diarrhea can result in a severe loss of blood proteins and body salts, otherwise known as electrolytes (potassium, sodium and chloride), into the bowel. Severe reductions in blood salts
(potassium in particular) can produce symptoms of profound weakness and unsteadiness on
the legs and may also interfere with the animal's heart rhythm and brain activity (strange neurological symptoms and even seizures can result). Severe loss of blood proteins can occur as a result of both inflammatory fluid loss and whole blood loss
into the bowel. Severely low blood protein levels can result in the fluid within the blood vessels (plasma) leaking out of the blood vessels into other areas of the body. This will result in a drop
in the animal's blood pressure (worsening shock) and, depending on where it settles out, the leaking
fluid can interfere with the function of other organs (e.g. fluid in the lungs can cause difficulty breathing,
fluid in the brain can result in brain dysfunction, seizures and coma).
5. Complications of coccidial infection: if colonic bleeding is severe.
Animals (especially young puppies and kittens) can bleed enough from coccidial induced intestinal ulceration that they become severely anaemic. Anemia is a condition whereby there is not enough
red blood cells in the animal's circulation to carry oxygen adequately around its body. These animals develop a rapid heart rate and respiratory rate and very pale to white gum
color (see images below). Left untreated, these animals can suffer severe tissue and organ damage
(e.g. brain damage and renal failure) from a lack of circulating oxygen and may eventually become
comatose and die. Lots of blood in the faeces, particularly in a young kitten or pup,
should be a big concern to owners and urgent veterinary attention is recommended.


Image 1: This is a dog with very pale gum color. Ignore the black/brown pigmentation
on the animal's gums and look at the spaces between the black spots - see how pale
and white they are? These regions should be a bright salmon pink colour. This is a
dog with severe anaemia.
Image 2: This is the feces (believe it or not) from a dog with very severe colitis. The diarrhoea is almost frank blood, aside from the whitish coloured flecks visible throughout
it (the white flecks are mucus chunks produced by the irritated colon).
6. Complications of coccidial infection: secondary bacterial infections.
The coccidial infection strips away the protective epithelial cells lining the intestines and colon, resulting in large ulcers that expose the more-fragile, underlying intestinal tissues.
These bleeding ulcers provide a perfect site for the nasty bacteria of the gut (including true nasties like Salmonella, E.coli and Clostridium) to
colonize and the large volumes of inflammatory proteins and secretions within the damaged bowel provide nutrition for the bacteria, allowing their populations to grow quickly. These bacteria are given plenty of opportunity to multiply and increase
in number because the damage to the intestine reduces and/or alters its motility, thereby allowing the bacteria to remain and grow in one site rather than
being moved on by normal gut motion. Once the bacterial population reaches significant numbers, these secondary bacterial infections
can start to cause bowel problems of their own. Bacteria release nasty toxins and bowel-damaging
chemicals that further injure the intestinal lining, worsen the diarrhea symptoms and
make the animal feel miserable, sick and feverish. Animals with severe secondary bacterial
infection may go off their food and can appear very unwell.
Author's note: These secondary bacteria can often be detected on fecal culture and seen on rectal or faecal swabs. It can be difficult for the vet, when confronted by
coccidia as well as intestinal bacterial pathogens, to know which organism
started the problem off (which came first). The bacteria could be the primary issue
and the coccidia just a secondary organism taking advantage of the bowel injuries to replicate or,
alternatively, the coccidia could be primary problem and the bacteria the secondary opportunists.
If the secondary bacterial infection progresses, eventually bacterial organisms and/or their bacterial toxins may enter the bloodstream, resulting in severe illness, septic shock and the potential for multiple organ infection/damage and even organ failure. These 'septic' animals are very weak and lethargic and are often febrile
(feverish). They are usually inappetent and may have even progressed to the point
of frequent, projectile vomiting. Their feet and faces will feel hot to touch and they will pant a lot. If they are not anemic, their gums will often take on a horrendous dark, brick-red to purplish colour: a result of fever, dehydration and septic shock
(in septic shock, the animal's peripheral blood vessels dilate inappropriately, dropping
the animal's blood pressure severely). Death will often be the result.
Circulating bacteria can become deposited into the small capillaries of the joints, eyes, heart
and kidneys, leading to infection of theses places. Septic arthritis (bacteria in the joints), in particular, is a well-known complication of parvo virus and many other nasty
ulcerative intestinal diseases in puppies and kittens.
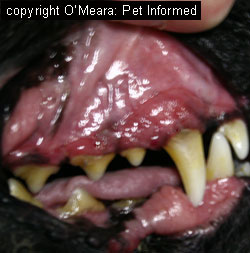
Image - these are the brick-red coloured gums of a dog with severe septicemia. This particular animal
had pneumonia, but could easily have had severe bacterial colitis or enteritis.
7. Complications of coccidial infection: intussusception and rectal prolapse:
Small intestines and colons infected with coccidia can become very thickened as a
result of severe ulceration and inflammation of the intestinal wall. The motility of the infected bowel is often abnormal: some parts of the intestine may be excessively hypermotile (moving too much in response to infection - trying to clear the infection) and other parts may be excessively hypomotile (not moving enough at all as a result of damage and inflammation). This abnormal intestinal motility can occasionally result in the coccidia-affected intestine or colon telescoping into itself, causing a complication caused an intussusception.
Sections of bowel trapped inside of other sections of bowel can result in severe rotting and damage of the intestine if left untreated. Correction of this complication requires surgery: surgery that is likely to be done on an already malnourished, possibly septic, and compromised animal.
In addition to intussusception, animals with severe colitis (including coccidiosis)
can sometimes develop a complication called a rectal prolapse. This is where the rectum
itself comes out of the bottom, like a large pink sausage. It occurs when animals
strain and strain to defecate as a result of colonic irritation - eventually this straining can result in the whole rectum coming out. Left untreated, the exposed rectum
can rot and die off, resulting in severe illness and, potentially, the death of the pet.
Surgery may be required to replace the rectum, should manual techniques fail to return it
to its correct place.



Image 1: This is an image of a young cat with a rectal prolapse.
Image 2: This is a close up of the prolapse, showing that it is coming out of the anus.
Image 3: This is an end-on view of the prolapse, showing the tunnel which is the
central canal of the colon.
8. Complications of coccidial infection: long-term, chronic infection and weight-loss (fading kittens and puppies):
The small intestine (the main site of coccidia invasion) is the main site of nutrient absorption and uptake in the animal body. Some kittens and puppies affected with coccidiosis do not become acutely and severely ill from dehydration and secondary bacterial infections,
as described above. Instead, some of these kittens and puppies develop a lower-grade, chronic, longer-term coccidial infestation of their small intestines which, although it does not rapidly kill them, causes enough small intestinal damage that they are unable to absorb their food properly. Unable to absorb their food properly, these chronically affected kittens and puppies will become malnourished and will steadily lose weight and condition.
They will become thin and underweight, with coarse, starey hair-coats and bony frames. Their faeces,
although not watery, will often be loose and soft with whole, undigested food particles
appearing in the droppings. These animals will often be ravenous (starving hungry) and
will eat everything they can get hold of and yet, despite this good appetite, they will keep losing weight. Many of these creatures will die as a result of chronic wasting (fading kittens and puppies) and as a result of increased susceptibility to other infectious diseases (malnutrition reduces their immune system defenses to all diseases).
4c) Chronic, recurrent coccidia infections - coccidia that keeps returning.
In the vast majority of cases of non-complicated coccidiosis, the antiprotozoal drugs and other therapeutics prescribed by the veterinarian will have their desired effect: the symptoms of coccidial infestation will abate and the puppy or kitten (or older pet) will be fine. In a smaller proportion of patients, however, the symptoms of coccidiosis will persist, despite
the treatment given. These symptoms may either completely refuse to go away at all, even during the
period of medical treatment, or they may go away for a period of time during and after treatment (during which time the animal will appear to defecate normally), only to reappear later, days to weeks to months down the track.
So what is happening here?
Well, there are many reasons why the symptoms of coccidiosis may persist or keep on recurring
within the one animal. These are as follows:
1) The primary disease is not coccidiosis (i.e. the symptoms of enteritis and colitis being treated are not being caused by coccidial organisms):
There are many disease conditions that can closely mimic the intestinal symptoms of coccidiosis.
The list is large and includes a wide range of parasitic diseases, bacterial diseases, viral diseases, inflammatory bowel conditions, structural intestinal and colonic diseases (bowel cancers etc.), constipation disorders, intestinal accidents (e.g. intussusception, volvulus)
and intestinal foreign bodies. Some of these diseases are very simple to diagnose and differentiate from each other using basic physical examination techniques (e.g. rectal examination can quickly diagnose constipation - the presence of
hard, impacted faeces in the rectum and colon) and/or basic diagnostic testing methods (e.g.
whipworm infestation can be easily diagnosed on fecal flotation if whipworm eggs are found), however, some of the causes of intestinal disease symptoms can be very difficult to diagnose by simple testing
methods alone. They need more advanced diagnostics. Making the task even more difficult for veterinary diagnosticians is the fact that
some of these intestinal conditions may even occur concurrently with other intestinal diseases,
such as coccidia, making the primary cause of disease symptoms tricky to determine.
Vets that fail to detect the 'more difficult to diagnose' intestinal diseases or fail to
recognize the presence of another, concurrent, primary disease condition, may easily misdiagnose an animal as having coccidiosis, particularly if a couple of coccidial
oocysts get seen in a fecal float.
As mentioned previously, coccidian oocysts can often be found in the faeces of normal dogs
and cats whose immune systems have never been 100% able to clear the parasite infection (i.e. the coccidia carrier state). These non-symptomatic carrier animals can become affected by another non-coccidian intestinal disease (e.g. inflammatory bowel disease (IBD), intestinal bacterial infections like Clostridium), develop symptoms of gastroenteritis
or colitis and be misdiagnosed as coccidiosis because the vet finds coccidia oocysts in
their faeces (see section 5). The fact is, these coccidia carrier animals would
have had the coccidial cysts in their feces even in the absence of any intestinal signs. Should the vet misdiagnose the animal as having coccidiosis and treat for that disease, it is very likely that the intestinal symptoms will persist. This is because the primary intestinal disease problem (e.g. IBD, bacterial infection etc.) has not been diagnosed or treated. As a result, the vet and owner will think that the coccidia
infection is persistent, when, in fact, the disease symptoms seen are due to something else entirely.
Even more confusing for vet and owner: because coccidia is not cleared from the intestine by most anticoccidial medicines
and because it is an organism that tends to replicate opportunistically in the presence of concurrent intestinal disease (i.e. it takes full advantage of a sick intestine), the next time that the patient appears to the vet with those same intestinal symptoms,
it is highly probable that coccidial oocysts will still be discovered in the faeces. This finding will serve to further convince the vet that the coccidia is the cause
of the problem, even when it isn't. The vet might even decide to trial a different
anti-coccidial medication this time around, however, no improvement will be seen. The intestinal problem and symptoms will persist, regardless of coccidial treatment applied, until the primary, non-coccidial, intestinal disease is found and sorted. Further work-up, including: rectal smears, fecal ELISA tests, abdominal radiographs (x-rays), abdominal ultrasound, colonoscopy and colon biopsy may be needed to find the
true cause of the symptoms.
2) The coccidial organism(s) diagnosed on fecal flotation are not the right kind:
 As mentioned previously, most coccidia species are host specific when it comes to the types of
animals whose intestines and colons they will infect. An oocyst belonging to a cat- or pig-adapted
coccidian organism will not hatch in a dog intestine and nor will it replicate to cause symptoms of intestinal disease in a dog. Instead, should a dog consume the droppings
of a coccidia-infected non-canine species of animal (e.g. a dog that regularly consumes pig poo or cat droppings),
any oocysts ingested will pass through the dog's intestines unhatched and come out, unharmed,
in the stools of that dog. A veterinarian who subsequently performs a fecal flotation on that dog's droppings may misdiagnose that dog as having coccidiosis should
he or she fail to recognize that the coccidial oocysts seen are not of the dog-infectious variety.
Similar to the situation described in point 1 of this section, symptoms of intestinal disease
seen in this kind of patient will not respond to coccidiosis treatment because the coccidian
organisms found in the stools are not the cause of the issue. The animal will continue to show abnormal intestinal symptoms (the coccidiosis will seem to 'persist') until the true
intestinal issue is diagnosed.
As mentioned previously, most coccidia species are host specific when it comes to the types of
animals whose intestines and colons they will infect. An oocyst belonging to a cat- or pig-adapted
coccidian organism will not hatch in a dog intestine and nor will it replicate to cause symptoms of intestinal disease in a dog. Instead, should a dog consume the droppings
of a coccidia-infected non-canine species of animal (e.g. a dog that regularly consumes pig poo or cat droppings),
any oocysts ingested will pass through the dog's intestines unhatched and come out, unharmed,
in the stools of that dog. A veterinarian who subsequently performs a fecal flotation on that dog's droppings may misdiagnose that dog as having coccidiosis should
he or she fail to recognize that the coccidial oocysts seen are not of the dog-infectious variety.
Similar to the situation described in point 1 of this section, symptoms of intestinal disease
seen in this kind of patient will not respond to coccidiosis treatment because the coccidian
organisms found in the stools are not the cause of the issue. The animal will continue to show abnormal intestinal symptoms (the coccidiosis will seem to 'persist') until the true
intestinal issue is diagnosed.
See image: The coccidian oocyst on the left is Isospora felis, a known pathogen of the cat. Finding lots
of these in a cat's dropping may be significant. The coccidian organism on the right is not Isospora: it could be a non-pathogenic cat-adapted organism such as Hammondia or
it could be a fecally-ingested oocyst from a non-cat species of animal that is just passing
through. Even though they look impressive, finding lots of these in a cat's droppings may not be significant at all.
In the case of a dog or cat that regularly consumes the faeces of other animals,
frequent symptoms of gastrointestinal upset and intermittent enteritis and colitis are more likely to be caused
by the animal's dietary indiscretions (eating garbage and rotten faeces) and/or nasty
bacteria present in the poo (Salmonella, E. coli, Clostridium, Campylobacter).
Diagnosing atypical coccidial species in the patient's droppings will at least give
the vet a vital clue that this animal is probably wandering and that it is scrounging
for droppings and probably other rotten foodstuffs and carcasses as well.
Fecal oocyst culture - see section 5c - is required in order to diagnose the species of coccidian oocyst present in the stools. Rectal smears and fecal bacterial culture can be used to diagnose bacterial pathogens that might be the cause of intestinal symptoms following fecal consumption.
3) You are dealing with a true coccidial infestation (i.e. not a misdiagnosis) that keeps on re-activating:
The re-emergence and re-activation of latent (dormant) coccidia infestations is the most common reason for prolonged (chronic) or recurrent symptomatic coccidian infections.
As mentioned previously, coccidian infestations do not tend to be completely cleared from the body by the host's immune system. In most animals, the coccidian organisms
and the host's immune system establish a balance whereby the coccidia are unable to replicate rapidly and
cause any disease signs in the host, but the host's immune system is unable to clear them from the body. This balance between host immune system and parasite can last for months to years without the dormant, latent coccidial organisms reactivating or
causing any clinical disease symptoms.
If the host immune system fails to maintain this balance, however, the coccidians can re-emerge, replicate quickly and produce disease symptoms in the host. Should the immune system recover quickly
(e.g. the immune system was only 'down' for a short while because of a brief period of intense stress), then that animal will recover and the coccidia will be forced back into a dormant state
with no more clinical symptoms. If, however, the animal's immune system is rendered ineffective for a long period of time (e.g. due to immune disease; long-term immune suppressant drugs; chronic, long-term stress situations), then the coccidia will persist and become a longer-term clinical problem. These animals will persistently display
symptoms of enteritis and shed coccidia in their faeces. The only time that symptoms may appear to abate in these animals is when those animals are being treated with antimicrobial drugs: the affected animals will seem to recover from the infection, only to relapse as soon as the drugs are discontinued. This relapse occurs because most coccidial antimicrobial drugs are unable to completely clear coccidia from the
intestines and because treated animals often soon get new infestations from a contaminated
environment.
Recurrent and persistent symptomatic coccidial infections can occur in animals that are exposed to a lot of stress - e.g. poor husbandry, conditions of extreme heat and cold, poor or imbalanced nutrition, concurrent illnesses, lactation, weaning or pregnancy, transportation, overcrowding, altered environment, re-homing, owner absence etc.
They can also occur in animals that have immunosuppressive diseases (e.g. immune mediated disease, diabetes mellitus, Hyperadrenocorticism (Cushings disease), AIDS, FIV (feline AIDS), FeLV (feline leukaemia virus), cancer, leukemia or congenital (genetic) immune disorders) or that are on immune suppressive medications (e.g. corticosteroids, chemotherapy drugs).
The work-up (diagnostic steps) of chronic and/or recurring coccidial infestations involves two vital steps:
A) rule out other causes of intestinal disease first: remember points 1 and 2 - symptoms of intestinal disease can be caused by a number of other intestinal disorders, commonly misdiagnosed as coccidiosis
AND
B) if coccidia is the only identifiable cause of the intestinal symptoms seen, determine whether
or not there is an underlying source of stress and/or immune suppression and remove it (if possible). Failure to remove any underlying immune suppression (including stress) will result in
the coccidia persisting and disease symptoms constantly reappearing.
4d) Coccidia diagnosed in adult dogs and cats - is it significant?
Significance of adult animals with coccidia symptoms:
The main time we vets tend to encounter clinical symptoms of disease caused by coccidian organisms
is in very young kittens and puppies, under 6 months of age (usually much younger - around 1-4 months of age). Young animals' immune systems are naive (have not been previously exposed
to the parasite) and their immune defense responses take time to adapt to the coccidial
infection and to suppress it. The time taken for the juvenile immune system to adapt to and respond to the new parasite infestation allows the coccidial parasites to get a head start with their replication and cell destruction - this is the reason why young animals are most likely to show clinical symptoms of coccidial disease. Although coccidial oocysts can often be found in the faeces of older animals, it is much more uncommon for adult animals to
actually show clinical symptoms of coccidial infection. This is because the immune system
of an adult animal has often 'seen' (been exposed to) the parasite before and, thus, is quick to deal
with it before the organism has a chance to replicate and cause disease symptoms. For the most part, coccidia ova (oocysts) found in the faeces of older animals, particularly animals showing no symptoms of disease, are not of much clinical significance at all.
An older animal (6-12 months or more) that has never before been exposed to coccidian organisms
may develop clinical symptoms of coccidiosis if it ingests the organisms from its environment.
Similar to the situation seen in young pups and kittens, these clinical disease signs would
occur because of the naive state of this adult animal's immune system and the time
taken for that immune system response to adapt and develop and respond appropriately. It would be expected that such an animal would display mild symptoms of
coccidiosis (probably not as severe as the disease seen in the very young) and shed lots of coccidial oocysts into its feces until its immune system kicked in and suppressed the infection, thereby resolving the clinical signs.
Although the situation described in the paragraph above (coccidia infection of
an immunologically naive adult animal) can indeed occur, it must be mentioned
that such an occurrence is relatively rare. Coccidia is such a ubiquitous, wide-spread
parasite that it is uncommon for most dogs and cats to get to adulthood without having
ever encountered it before. Consequently, I would always interpret a diagnosis of clinical coccidiosis in an adult animal with some degree of caution. Clinical coccidiosis is really not that common in adult animals, particularly animals that have previously had the
disease in kitten-hood and puppy-hood, and, although I would certainly
treat for the condition if I found it on a faecal float, as a veterinarian I would always
keep at the back of my mind the possibility that this animal could just be a coccidia carrier (always
asymptomatically shedding oocysts) with some other colonic or intestinal disease causing the symptoms
seen. Alternatively, if that adult animal did indeed seem to have a true case of coccidiosis (heaps of oocysts in the poo, supportive clinical signs etc.), I would
always consider it a possibility that this animal could have an underlying stressor or
some other immune suppressive disorder making the parasite appear and cause disease. My suspicion of an underlying immunosuppressive process would be increased further should this animal go on to show repeated bouts of clinical, symptomatic coccidiosis.
Significance of adult animals as coccidia carriers:
As mentioned previously, adult animals with no clinical symptoms of coccidiosis
(the animals are termed carriers) will often be found to have low numbers of coccidial oocysts in their faeces on a faecal float. Although this subclinical coccidia infestation is unlikely to be of clinical disease significance to that carrier animal (we don't even recommend
medical treatment for it), it must be re-iterated that this non-clinical shedding of oocysts into
the faeces is of significant risk to young, susceptible animals. Young animals that
consume these faeces will ingest the oocysts and are likely to show significant symptoms of disease compared to their adult carrier counterparts.
In order to reduce the spread of coccidiosis to young, susceptible, immunologically
naive animals, adult carrier animals should not be housed in the same pens or runs as underage animals (under 6 months). This is particularly important if coccidia
is to be ever controlled in large, multiple dog or cat facilities such as boarding kennels, catteries, breeding facilities, pet-shops and vet clinics.
Carrier animals also pose a risk to immunosuppressed older or younger animals. Animals
on chemotherapy or that have immune system disorders or high, long-term stress levels
may develop clinical signs of coccidiosis, should they consume the organisms from
a carrier animal's stools.
Author's note: The clinical significance of any coccidial infestation, be it in older animals or younger animals, must take into account the species of coccidian oocysts discovered. Hammondia, Besnoitia and Sarcocystis oocysts are generally of little clinical significance to the definitive host - these organisms
do not usually cause significant intestinal disease or intestinal signs in the dog or cat. Finding the oocysts of non-dog and non-cat species of coccidian organisms in a dog or cat's faeces
tells us that the dog or cat has been eating the infected poo of other animals, but that coccidiosis is not the cause of any intestinal upsets seen (atypical coccidia oocysts simply move through the intestines of the dog and cat without hatching or replicating).
4e) Can animals be infected with coccidia and show little or no signs of disease?
This has pretty much been discussed in sections 4a and 4d, but I will summarize it here.
Animals that have previously recovered from coccidial infestation (regardless of whether they received
antimicrobial medications or not) will often go on to develop a coccidia carrier
state. A carrier state means that these animals are still infested with the organism
and still intermittently shed the infectious organism oocysts in their faeces, but they
show no clinical signs of disease. The carrier state develops because the animal's immune system
response to the organism is enough to suppress the organisms' rapid growth and replication
in the gut, but not enough to clear the organisms completely from the body (the organism hides out
inside of the animal's intestinal epithelial cells, thereby avoiding the immune system's destruction).
Carrier animals pose a huge risk to young, susceptible animals and immunosuppressed or
stressed animals because they shed infectious oocysts into their faeces, which might be
consumed by such animals. Carriers are a massive problem in multiple-dog or multiple-cat facilities
because they are difficult to identify and isolate from the rest of the population and because they constantly shed the resistant oocysts into the environment. Treating
coccidia infected puppies and kittens costs such businesses lots of money, as does the staffing
and chemical control (disinfectant) methods needed to combat and manage the disease.
4f) Sarcocystis neurona - equine protozoal encephalomyelitis.
Sarcocystis neurona is a parasite of the alimentary tract (gastrointestinal tract)
of opossums that can invade the tissues and organs of a range of intermediate host species,
including cats, horses and a number of wild animal species. When the infectious, fecally-shed oocysts are ingested by a horse or cat or wild animal, the protozoan tachyzoites
invade and replicate rapidly within the brain cells of that animal, producing severe, often fatal,
neurological disease symptoms. The infected animal may display a range of different, progressive neurological signs including: wobbliness, incoordination, lameness, paralysis, muscle wasting and fecal and urinary constipation or incontinence.
Seizures, coma and death may be the end result. The disease condition is well-known in American horse facilities, where it is termed equine protozoal encephalomyelitis.
The disease is only just being recognised in cats and is not so well-known in this species.
Diagnosis of the disease in horses is generally achieved by detecting an increased level of S. neurona antibodies in the cerebrospinal fluid (CSF) of the infected horse using Western Immunoblot techniques. PCR, specially designed for the amplification and detection of S. neurona DNA,
can also be used to detect the organism in the CSF samples of cats and horses. Only a few specific, diagnostic laboratories are equipped to run these tests. If the patient happens to
die from the disease, diagnosis can also be made postmortem by the histological examination of
the animal's brain tissues - tachyzoite and bradyzoite cysts can be easily seen in infected braincells.
Treatment of S. neurona infection is not always successful, but attempted medical protocols in horses include:
Pyrimethamine at 0.1-0.25mg/kg once daily for 4-12 weeks in conjunction with 7.5-10mg/kg
twice daily trimethoprim sulfonamide antibiotics. Trimethoprim sulfonamide drugs access the brain tissues and CSF of animals quite well, making them very useful for protozoan brain diseases.
Ponazuril, a close relative of Toltrazuril, has also been trialled successfully in horses
with equine protozoal encephalomyelitis.
At the moment, management and treatment of the feline form of Sarcocystis neurona infection
has to be extrapolated from equine drug dosing regimens. The disease is relatively
new in the cat medicine world and more study needs to be done on it before optimal
medical regimens are able to be recommended.
Author's note: Sarcocystis neurona has been known to cause severe neurological
disease symptoms in skunks and raccoons. These particular wild animal species are also known to be common carriers of rabies and distemper - viral diseases which also produce neurological symptoms. Rabies is a very dangerous disease to man and wild animals with neurological disease signs should never be approached. Don't make the mistake of
assuming that neurologically affected skunks and raccoons have S. neurona - always treat them as possible rabies carriers and keep well away! See our comprehensive rabies page for more on rabies disease, treatment and prevention.
This disease condition is most 'common' to the USA and places that have opossums. As far as I can tell, the condition is exotic to Australia - Australia has possums, but not the
kinds of possums (opossums) that are encountered in the United States of America.

5. How is coccidiosis diagnosed? - Testing for coccidia.
Coccidiosis is routinely diagnosed using an in-house test called a faecal flotation test
(also known as a Fecalyzer test or fecal float test). The aim of this simple test is to detect
coccidial oocysts (the infectious forms) in the stool samples of infected definitive host
animals (e.g. dogs and cats). Other supportive diagnostic tests, including: fecal smears (wet preps), fecal oocyst cultures and intestinal biopsies, may also be required in order to make a diagnosis or add to a diagnosis of coccidiosis.
5a) Fecal flotation.
 Faecal flotation is a test performed on the faeces of the clinically infected or carrier dog and cat, or any other animal species that is a definitive host for some species of intestinal coccidian. The test is performed in order to detect the presence of tell-tale coccidial oocysts in the faeces
of the infected animal, thereby supporting a diagnosis of coccidiosis. The test can also
be used to detect the fecally-shed oocysts of certain other parasitic protozoan organisms, including Toxoplasma, Cryptosporidium and Giardia, as well as the eggs of various parasitic worms, including whipworm, tapeworm, roundworm and hookworm.
Faecal flotation is a test performed on the faeces of the clinically infected or carrier dog and cat, or any other animal species that is a definitive host for some species of intestinal coccidian. The test is performed in order to detect the presence of tell-tale coccidial oocysts in the faeces
of the infected animal, thereby supporting a diagnosis of coccidiosis. The test can also
be used to detect the fecally-shed oocysts of certain other parasitic protozoan organisms, including Toxoplasma, Cryptosporidium and Giardia, as well as the eggs of various parasitic worms, including whipworm, tapeworm, roundworm and hookworm.
What the fecal flotation test entails:
The fecal float test involves mixing the faecal sample in a suspension of sodium nitrate solution (Sheather's sugar solution or zinc sulfate solution may also be used) using a special apparatus called a Fecalyzer (or Fecalyser). The faeces (which are heavier than sodium nitrate and the other solutions) sink to the bottom of the solution and the parasitic worm eggs and
protozoan oocysts float to the top of the solution. These eggs and oocysts gather
underneath a microscope coverslip (a small square of glass placed on the top layer of the solution), which is later (after 10 minutes) placed on a microscope slide (a large rectangle of glass) for examination under a microscope. The veterinarian then examines the slide under the microscope, looking for obvious worm eggs and protozoan oocysts.
The image on the right is of a fecal float that was performed on the feces of a kitten
with diarrhoea. The test revealed lots of coccidian organisms.
For an excellent step-by-step guide to in-house faecal flotation, see our great
faecal float page. The page contains great step-by-step pictures and photo images of how the test
is performed and what is seen under the microscope.
Collecting the faecal sample:
As a general rule, the best stool samples to perform a fecal floatation on are those that
are as fresh and recent as possible (i.e. straight out of the dog or cat). Ideally, feces
should be tested within 30 minutes of leaving the animal. The reason we want an extra fresh stool sample is because the eggs of some parasites (e.g. parasite worms) hatch very rapidly, making these parasites impossible to diagnose on aged stool samples. A fresh sample makes these parasites easier to detect. In the case of coccidia, the oocysts do remain viable for long periods of time and may be detected even in older poo samples (samples 1-2 days old), however, as a general rule: it is always best to go for fresh samples.
The veterinarian
will often collect an extra-fresh stool sample from your dog or cat's anus during the consult, using a gloved finger, or collect samples of faeces that your dog or cat passes in the consultation
room or cat carrier. Alternatively, you, as the owner, can help your vet to get a diagnosis by
bringing your pet's most recent stool sample (e.g. diarrhea sample) into the consultation for flotation.
Abnormal stool samples can even be dropped off at veterinary clinics for fecal flotation,
if owners are concerned about parasites in their pets. Although it is always recommended
that owner and pet go into the clinic for a proper consultation and examination,
busy owners on their way to work or owners unable to get an appointment until later
may attempt to get a more rapid diagnosis by dropping off samples of slimy, blood-tinged or diarrhoeic faeces for testing.
Fecal samples should be submitted in small, preferably sterile, air-tight containers such as fecal
sample jars or urine specimen pots, with the lid screwed tightly into place. Your vet can provide you with an appropriate specimen container to collect your pet's faeces into. At a pinch, you can use a new, ziplocked, sandwich bag for carrying faeces into the veterinary clinic - just make sure you double-bag the sample so that it does not leak. Do not use old
jam jars - even when cleaned, these contain fungi that can confuse the diagnosis.
Owners should always wear disposable gloves when collecting faeces. Faecal samples should be sent in to the vet as soon as they are collected, however, if the sample is collected
after-hours, you can place the well-sealed sample in the fridge for safe storage. Chilling the sample slows the development and hatching of any eggs and keeps the sample
fresh. Do not put samples in the freezer.
Pitfalls of faecal flotation - false negative results:
It is possible for an animal to truly have coccidiosis, but for tell-tale coccidial oocysts not to be found on a fecal floatation test. These test results are termed false negative test
results and they occur for several reasons:
1) Coccidial oocysts can be shed intermittently - many species of intestinal protozoa, including
Isospora, many other coccidians and Giardia, are well known for having a cyclic pattern
of protozoan replication and oocyst production. These organisms tend to release oocysts into the animal's faeces in waves. The consequence of this is that some stool samples will, therefore, contain loads of oocysts and others, from the same animal, will show almost none. Any vet, who happens to be unlucky enough to get the stool sample without organisms,
will come up with a negative result (a false negative), when other stools samples from the same animal might be full of the tell-tale oocysts.
2) Some coccidia shed very low numbers of oocysts - it is possible for an
animal to have clinical signs of coccidiosis and to only be shedding low numbers of
coccidial oocysts into the faeces. Oocyst numbers are not a reliable indicator of whether the
animal is clinically infected with the disease or not. Obviously, large numbers of
oocysts are most supportive of clinical infection, however, low numbers of oocysts
may be all that are seen in some animals as an indicator of active infection. Because
fecal floatation is performed using a human eye, it is possible for very small numbers of oocysts to be missed, if the vet isn't careful and observant, thereby resulting in a false negative result.
3) Lab error and veterinarian inexperience - fecal float examination is a
skill acquired with years of practice. It is possible for inexperienced practitioners
not to recognise parasitic oocysts and eggs and to make a false negative diagnosis.
4) Destruction of the parasitic eggs or oocysts by the fecal float solution - Some of
the solutions used in the fecal flotation process (e.g. sodium nitrate and sometimes even Sheather's Sugar solution) can distort or destroy the larvae, eggs or oocysts in the fecal sample, resulting in false negative results. Sarcocystis, as one example, undergoes complete maturation and
sporulation (matures to the infectious oocyst form) inside the dog or cat intestine - the
infectious oocyst that results generally breaks apart during fecal flotation procedures, resulting in false negative results. Zinc sulfate solution is thought to distort
and destroy oocysts, eggs and larvae the least of any of the flotation mediums and is
the medium of choice for Giardia and heavy eggs like Whipworm. Sheather's sugar solution
is preferred for coccidia, but will distort Giardia beyond recognition.
5) Certain parasite eggs do not float very well - some parasite eggs (e.g. whipworm) do not
float well on the typically-used fecal float solution: sodium nitrate. This can result in
false negative results (eggs that don't float can't be detected). Different floatation solutions (e.g. zinc sulfate) are required to diagnose them. Sodium nitrate is usually fine for diagnosis of coccidiosis (most coccidia float very well).
6) Some coccidial organisms produce severe enteric signs before the oocysts actually appear in the poo - it can take up to 11 days (15 in some species), from the time of infection, before fecally-shed oocysts will begin to
appear in the host's faeces, in order to be detected by a fecal float. Within this time, severe clinical
symptoms of coccidiosis can occur, without there being any oocysts visible in the droppings.
Pitfalls of faecal floatation - false positive results:
It is possible for coccidial oocysts to be found on fecal floatation and for
the animal not to actually have coccidiosis as the main disease process. These test results are termed false positive results and they occur for several reasons:
1) The animal is a non-clinical carrier - many animals, particularly adult animals, can develop a coccidia carrier state, whereby the organism is replicating slowly within
the intestines and shedding oocysts into the faeces, but not actually causing any clinical symptoms. If these carrier animals develop symptoms attributable to intestinal or colonic disease, the vet is very likely to find coccidial oocysts on a faecal floatation test, without the coccidia
actually being the cause of disease! This will result in a false positive result.
Treatment directed at the coccidia is unlikely to resolve the symptoms of disease because the primary intestinal disease has not been diagnosed or treated.
2) The animal has clinical coccidiosis due to an underlying immune disorder - this is kind of a true positive/false positive situation. Carrier animals with coccidia
in their intestines can revert back to clinical signs of coccidiosis if their immune
system control over the coccidia organisms in their bowels fails. This can occur due
to stress or many other congenital and acquired immune deficiencies. Although
finding coccidia oocysts in the faeces of these animals is proof of the coccidian infectious disease causing the symptoms (a true positive), it can also be considered to be a false positive, if the underlying immune disorder or stressor that is causing the coccidia to become a problem is not diagnosed and managed too.
3) The coccidia species is not the right species for that host - as mentioned
previously, dogs and cats that eat the droppings of other animal species can consume
oocysts that will travel, unchanged, throughout the dog or cat's intestines and be shed
into their faeces. Vets that fail to recognise these oocysts as non-dog and non-cat species
of oocysts will incorrectly diagnose these animals as positive for the disease.
4) Lab error and veterinarian inexperience - lots of weird objects can be found in
fecal floats: anything from pollen balls to fungal elements. It is possible for inexperienced vets to incorrectly identify these objects as parasite oocysts and to, therefore,
determine the animal to be positive for the disease.
5b) Fecal smear (wet prep).
A fecal smear, otherwise known as a wet prep, can be a very useful, simple test for detecting
certain parasites in extra-fresh fecal samples and rectal swabs.
The test involves taking a very small
sample of feces or colonic-mucus and breaking these faeces/mucus-samples up on a microscope slide using some saline solution (0.9% NaCl - sodium chloride). A coverslip (a tiny square of glass) is placed on top of the faeces-saline mixture and the sample is examined under a microscope for parasites. That's it! How easy!
Wet preps are valuable, simple diagnostic tests that can be used to detect a whole range of
parasitic organisms not easily detected on a fecal float. Motile (swimming) organisms
such as Giardia and Trichomonas, that are normally destroyed by fecal
float solutions, are not destroyed by saline and, thus, may be diagnosed on fecal smears. Similarly, many other oocysts and worm larvae, normally destroyed or severely distorted
by fecal flotation mediums, are not distorted by saline and, thus, may be detected on
fecal smears. Heavy eggs, such as whipworm eggs, may also be found on fecal smears because
fecal smears do not rely on floatation techniques.
Despite their good qualities and ease-of-use, fecal smears should not be considered
to be a complete replacement for fecal floatation techniques. Fecal smears come with
a major drawback: because such a tiny sample of feces or mucus is used in this test, only highly-numerous organisms that are diffusely distributed throughout all of the faeces are likely to be detected. Fecal floatation is a much better technique for detecting
smaller populations of organisms because greater volumes of faeces can be floated.
The two tests should be thought of as supportive of each other - each having their own
strengths and weaknesses. The two tests should be used in conjunction with each other
in any animal with symptoms of intestinal disease.
5c) Fecal oocyst culture.
The species of coccidian oocyst found in a fecal sample is generally determined by observing the
oocyst in its fully-matured state and counting the numbers of sporozoites (infectious protozoan
organisms) and the number of sporocysts (compartments holding the sporozoites)
within that mature oocyst. Because it takes time for oocysts in the faeces to mature to
their infective forms (whereupon the species of coccidian is determinable), veterinarians
and pathologists need to wait for a few days before the fecally-shed oocysts can be identified.
In order to enhance the chances of obtaining a definitive oocyst species diagnosis, the vet or pathologist usually performs a fecal oocyst culture: placing the oocyst-infected faeces into optimum conditions of temperature and moisture so that the oocysts have the best chance possible of maturing into their infective, identifiable stages. To perform an oocyst
culture, oocyst containing faeces (as determined on a fecal float) are placed into a Petri dish containing a solution of 1% potassium dichromate. Only a shallow suspension of feces and potassium dichromate is placed into the dish because the organisms need the oxygen, diffusing into the suspension, to grow. After 2-4 days of incubating at room temperature, most of the coccidial organisms in the culture sample will have sporulated (matured) and should be identifiable
on a repeat fecal float.
5d) Colonic or intestinal biopsies.
Taking biopsies of the small and large bowel and sending these biopsy samples off to a laboratory for histological assessment (assessment of the intestinal cells, inflammatory cells and the overall intestinal tissue architecture/structure) is not commonly done just for the purposes of diagnosing coccidiosis. Because it is an invasive procedure, intestinal biopsy is normally only performed when fecal flotation and other less-invasive methods of testing (e.g. rectal smears, abdominal radiographs, abdominal ultrasound)
have failed to determine a complete diagnosis for an animal's gastrointestinal symptoms.
Many diseases, including: intestinal cancer, inflammatory bowel disease, bacterial
infections, protozoan infections, worms and intestinal viruses, can be diagnosed
by intestinal biopsy. In difficult-to-diagnose cases of coccidiosis, bradyzoite and tachyzoite protozoan clusters (the asexually replicating coccidia organisms) can sometimes be seen inside affected intestinal epithelial cells, on tissue biopsy sections. Free-living coccidial organisms (the protozoans that are located outside of the intestinal cells, looking for new cells to invade) can often be seen in biopsied regions of severe intestinal ulceration
(places where the epithelial cells have fallen away): organisms are clearly visible amongst the damaged cells and cell debris. In the case of coccidiosis diagnosis, multiple areas of the intestine and colon need to be sampled because the coccidial organisms may only
invade a few, localised sections of intestinal wall.
How to take the biopsies:
Biopsies of the stomach, upper small intestine (duodenum) and colon can be taken from
inside the intestine or stomach using endoscopy or colonoscopy (cameras inserted along the intestine, via the mouth or anus entry-points) and biopsy forceps (small clamps that
bite off samples of the intestinal or colon lining). Alternatively, biopsies of
any section of intestine (as well as other organs such as the liver, pancreas and kidney) can be taken by opening up the animal's abdomen and sampling the organs from inside of
the abdomen (this procedure is called an exploratory laparotomy ('ex lap') and biopsy). Exploratory laparotomy is often superior to endoscopic biopsy procedures because, although it is more
invasive, it allows the vet to clearly visualise the entire abdomen; selectively biopsy
the regions of the intestine that look most diseased (and which are, thus, more likely to yield conclusive, diagnostic results); biopsy all layers of the intestinal wall (endoscopy only takes the intestine lining, not all layers of the intestine) and identify specific lesions (e.g. focal intestinal cancers) that might not be seen on endoscopy.
5e) Additional testing - when coccidia can not be found.
Coccidiosis is only one of the diagnoses that might be made in an animal that presents
with symptoms of enteritis, colitis and intestinal disease. Usually, if an animal truly does have coccidiosis as the cause of its diarrhea and colitis symptoms, then fecal flotation, fecal smears and/or intestinal biopsy should be ample to diagnose it.
As will be discussed in the next section (section 6), however, there are many diseases which can produce symptoms of intestinal disease, similar to coccidiosis. Although many of these other non-coccidial diseases can also be diagnosed using the testing procedures already mentioned (fecal float, fecal smears, colonoscopy, exploratory laparotomy and intestinal biopsy), some of these differential diagnoses alternative diagnoses)
need special tests to diagnose them. These specific diagnostic tests will be discussed in detail on the
pages relevant to the disease processes in question but, for completeness, I have mentioned
some of these alternative tests here.
Fecal smear: a moist cotton tip is rubbed on the animal's rectal wall lining, just inside of the animal's anus. The cotton tip is then rolled onto a microscope slide (making a 'smear' of feces and rectal-lining cells
on the slide) and the slide is dried and stained in special stains. Once dry, the slide is examined under a microscope for the presence of diagnostic intestinal cells,
inflammatory cells, bacteria and other organisms. Organisms such as Clostridium
infection, Campylobacter and Giardia infection can be found on rectal smears, along with
diseases such as inflammatory bowel disease (not as accurate as biopsy though) and occasionally
even intestinal lymphoma.
Images of rectal smears seen under the microscope:
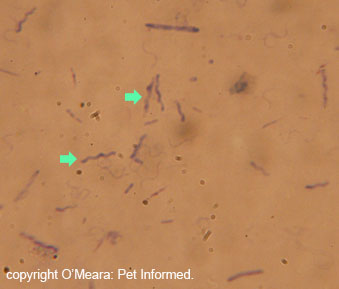
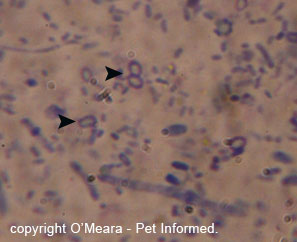

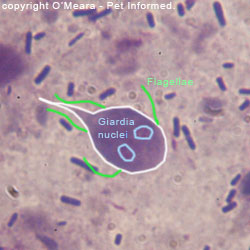
Image 1: This is a fecal smear of Campylobacter organisms as seen under a microscope.
The Campylobacter are the wiggly zig-zag lines marked with green arrows: they are often described as being shaped like flying birds (seagulls). These particular
organisms came from a puppy with severe, mucussy diarrhea and bright red blood in the faeces. Note
that, because other non-Campylobacter, spiral-looking organisms can sometimes be found in the faeces of
animals, Campylobacter should always be confirmed using a fecal bacterial culture (next point).
Image 2: These are Clostridium spores (the white-filled circles marked with arrows) taken from a rectal swab of a dog with diarrhoea. This animal had symptoms of colitis
after eating roast lamb.
Images 3 and 4: Giardia. The outline of the organism, along with its tail is marked in white.
Its paired nuclei are marked in blue. Its flagellae (small 'hair-like' structures that it swims with) are marked in green.
Fecal culture: feces can be cultured at the laboratory to detect whether they contain
pathogenic (disease-causing) bacterial types such as Campylobacter, Salmonella
and Yersinia.
Fecal ELISA: ELISA tests are advanced testing procedures used to detect the presence
of specific organism antigens (proteins) in fecal samples. Fecal ELISA tests have been developed for parvovirus and coronavirus infections, as well as for Giardia and Cryptosporidium:
two parasitic organisms that are notoriously difficult to detect using normal fecal assessment techniques.
Fecal ELISA tests have also been developed to detect nasty tapeworms like Echinococcus (hydatid tapeworms).
Fecal PCR: PCR is a highly-advanced technique for detecting the presence of specific parasite or infectious organism DNA in tissue and fluid samples. It is highly sensitive and able to detect very small amounts of any organism. PCR tests have been developed for Giardia and Cryptosporidium: two organisms that are notoriously difficult to detect using normal fecal assessment techniques.
Serology - antibody detection: when an animal
becomes infected with an infectious organism or parasite, its immune system produces specific
antibodies designed to enhance the killing and clearance of that organism from the animal's body.
These antibodies can be detected in the animal's blood and may be used to make a diagnosis of a specific
infectious disease organism. Antibody detection tests have been designed for many infectious
disease organisms, including: Toxoplasma, Neospora, S. neurona.

6. What other diseases look like coccidiosis in dogs and cats?
Coccidiosis is characterized by irritation and inflammation of the small intestine and sometimes the colon, resulting in symptoms of enteritis and colitis: watery to semi-solid diarrhea; slimy, jelly-like stools; stinky,
putrid-smelling stools; fresh blood in the faeces; increased frequency of defecation; straining to defecate;
dehydration and occasionally weight-loss, wasting, weakness, pale gums and vomiting.
Sounds simple enough ...
Unfortunately for those of you who like to self-diagnose, there is a wide range of other conditions that dogs and cats can get which may also present as symptoms of intestinal disease. Basically, any condition that causes severe irritation or inflammation of the small intestine and colon will produce these clinical signs. The following
is a list (by all means not exhaustive) of conditions that can present similarly:
Inflammatory Bowel Disease (IBD) - a common, allergy-initiated, auto-immune condition whereby inflammatory
white blood cells (lymphocytes, plasma cells and/or eosinophils) attack the walls of
the intestines and colon resulting in symptoms of gastroenteritis and colitis. Proteins
from the animal's food or proteinaceous bacterial antigens are thought to be the underlying cause.
Whipworm - Whipworms (Trichuris vulpis) live in the colon, sometimes producing
signs of colitis.
Intestinal worms - Round worms, hook worms and tape worms live in the small intestines
of dogs and cats, sometimes producing symptoms of gastroenteritis in young animals (weight loss, diarrhoea, wasting).
Bacterial overgrowth - certain species of bacteria (especially Clostridium and E. coli species)
live in the intestines all of the time without causing any disease issues. They normally only become a problem when their numbers are permitted to grow out of control. This generally occurs when the animal is allowed to gorge itself on rich foods (e.g. lamb and pork are huge culprits) or ingest fouled garbage (stuff from the
bin, semi-rotten, spoiled foodstuffs, animal carcasses).
Bacterial pathogens Some bacterial organisms preferentially invade the intestines and colon,
causing signs of gastroenteritis. These include: Salmonella, Yersinia, Campylobacter and Clostridium. These organisms infect dogs and cats through the consumption of another animal's faeces or through the consumption of old/aged, undercooked or contaminated foodstuffs (e.g. food poisoning).
Giardia and Cryptosporidium. - semi-common, fecally-ingested protozoan organisms that can produce
a range of intestinal symptoms. The organisms usually come from contaminated waterways.
Viral enteric diseases. nasty intestinal viruses such as canine parvovirus, feline panleukopenia, canine distemper, canine coronavirus and rotavirus can produce symptoms
severe gastroenteritis: vomiting, diarrhoea, weightloss, abdominal pain, dehydration, bloody stools etc.
Diet changes - abrupt diet alterations, particularly in young animals, can commonly
produce symptoms of gastrointestinal upset - vomiting, diarrhoea, inappetence etc.
Intussusceptions - the intestine of some animals can telescope inside
of itself, producing symptoms of straining to defecate, blood in the stools, vomiting, inappetence,
weightloss and slimy droppings. Diagnosis is made by ultrasound, colonoscopy or exploratory surgery.
Constipation - constipated animals can present with signs of straining, bloody discharges from the rectum and anus and slimy, jelly-like anal discharges.
Intestinal masses - animals with intestinal, colon, rectum and anal cancers can present with signs of diarrhea, weight loss, straining to defecate, bloody discharges from the rectum and slimy, jelly-like anal discharges.
Intestinal foreign bodies - animals with intestinal, colon, rectum and anal foreign bodies can present with signs of vomiting, inappetence, weight loss, straining,
bloody discharges from the rectum and slimy, jelly-like anal discharges. Common foreign bodies include cooked bones, corn cobs, stone-fruit pits and pieces of
ingested stick.

7. Coccidiosis Treatment - how is coccidia in puppies and kittens and adult animals treated?
Most cases of coccidiosis in dogs and cats that present to a veterinary clinic are relatively non-complicated
cases. The puppies and kittens are bright and alert and interactive and normally still
eating, but they are producing vile-smelling, watery, slimy-looking stools; defecating more often than normal and occasionally producing flecks of blood in their droppings. Most of these non-complicated cases will be treated at home, using anti-coccidial remedies (section 7a), antibiotic-type medications (see section 7b) and dietary management (7e).
Occasionally puppies and kittens will present to the vet in a more critical state, with inappetence, weakness, severe dehydration and even anaemia and shock. These animals will
need to be cared for more intensively and often need to be admitted into hospital for
intravenous fluid support (7c) and even blood transfusions, in addition to the other treatment
modalities mentioned above.
As a general rule, the treatment of canine and feline coccidiosis is pretty much a treatment of the organism itself and management of its associated symptoms. The aim of therapy is to keep the animal comfortable, provide treatments that will kill off
most of the coccidia organisms and manage and prevent any secondary complications that might occur
(e.g. secondary bacterial infections, dehydration, anaemia, rectal prolapse). The hope is that, eventually, the animal's own immune responses will take over and control the coccidia's numbers
and replication, thereby bringing the condition to a conclusion. The treatment options for coccidiosis, their mechanisms of action and their pros and cons are discussed below.
7a) Antimicrobials - coccidiostats (drugs that inhibit coccidial growth).
Anticoccidial medicines are pretty much the mainstay of coccidia treatment. These
medications are designed to reduce the numbers of coccidial organisms present within the
animal's intestines and, therefore, reduce the damage that they are able to cause whilst the
animal's immune system is attempting to take back control of the situation. Although some
coccidial medications may occasionally clear coccidia from the gut completely, most coccidial
medications really only buy the animal time. Few of them completely eradicate the coccidial organisms
from the intestines - they just keep the bugs at bay whilst the immune system is
re-establishing the balanced state (premunition) between the host animal and the organism (the non-clinical carrier state). It is thought that these drugs may well
speed up the onset of premunition and shorten the symptomatic period of disease.
A lot of vets only prescribe anti-coccidial remedies to their 'well' coccidia patients and nothing else. Puppies and kittens that present to the veterinarian with diarrhoea
and abnormal faeces, but which are otherwise bouncy and bright and eating - these animals often do perfectly fine on anti-coccidial medications alone.
Animals that present to the vet with lots of blood in their stools, reduced appetites
and severe dehydration often require treatments in addition to anticoccidial medications
(e.g. antibiotics, fluids).
An important note on treatment: when dealing with litters of young puppies or kittens, do not only limit treatment to the sick creatures. Treat the whole litter and any other
underage animals that have come into contact with them. You can expect transmission to
have occurred.
Older animals that test positive (on a fecal float) for coccidia, but which have no
clinical signs of the disease do not need to be treated. These animals are probably immune
to the disease, but are non-clinical carriers. Treatment won't stop their carrier state
so treatment is not really worth it.
Commonly used coccidiostats (anti-coccidial drugs) include:
1) Trimethoprim sulfonamide combinations (trade names include Tribrissen, Trivetrin):
 Trimethoprim and sulfonamide are two individual antibiotic drugs that have been found to have
synergistic properties (enhanced organism killing properties) when they are used together. These drugs are the first choice (drugs of choice) for coccidiosis treatment
and are thought to be less toxic than many of the other antimicrobial chemicals used for this purpose.
Trimethoprim and sulfonamide are two individual antibiotic drugs that have been found to have
synergistic properties (enhanced organism killing properties) when they are used together. These drugs are the first choice (drugs of choice) for coccidiosis treatment
and are thought to be less toxic than many of the other antimicrobial chemicals used for this purpose.
In addition to suppressing coccidial growth and replication, trimethoprim sulfa
drugs are also able to kill many of the intestinal bacterial types that come in
secondarily and complicate coccidial infections. These include: Streptococcus, Staphylococcus, E. coli, Klebsiella, Clostridium, Proteus and Salmonella. They have poor action against Pseudomonas. The trimethoprim-sulfa drugs are particularly useful because they are able to access many tissues (including the brain) that many other antimicrobial combinations can not reach.
Some cautions: trimethoprim/sulfonamide (TRMS) drugs should be avoided or used very cautiously in very young animals, very old animals, animals with kidney issues and in very dehydrated animals because they have the potential to cause renal problems (crystals of TRMS will deposit in the kidneys, leading to renal injury).
TRMS has the potential to cause dry-eye (keratoconjunctivitis sicca - KCS) in susceptible individuals
and caution should be exercised, particularly in KCS-prone breeds like cocker spaniels
and cavalier king Charles spaniels. Trimethoprim/sulfonamide combinations should be avoided
in certain breeds, especially the dobermann and weimeraner, because of the risk of drug
induced autoimmune joint disease and skin disease.
Dose rate: 15-30mg/kg orally, once to twice a day if the pet is a cat or a dog under 4kg. Two references [23,25] suggested a dose rate of 15mg/kg twice daily for cats.
Dose rate: 30-60mg/kg orally, once a day if the pet (dog) is over 4kg. Note that the 4kg specification was only mentioned in a single text [ref 2] and that most other textbooks referenced here mention only the 15-30mg/kg dose rate (regardless of weight).
The trimethoprim-sulfonamide combination is generally administered for 5 days [ref 2, 22, 23].
According to Nelson and Couto [ref 1], the drug may be given for 10-20 days.
Another reference suggested giving the drug for 5-20 days, the length of time being
dependent on the animal's condition. The suggestion was to treat until the animal's
clinical signs had abated and/or until no oocysts could be detected in the faeces on fecal flotation. This would seem to make most sense from a veterinary perspective.
2) Furazolidone:
Furazolidone is a nitrofuran drug (nitrofurans are another antibiotic drug family) that can be used to treat coccidiosis, either on its own or in combination with the trimethoprim sulfa drugs.
Dose rate: 8-20mg/kg orally, once to twice a day (cat or dog) [ref 2,23,29,31] .
It is generally administered for 5-7 days.
Halve the dose when using furazolidone in combination with the trimethoprim sulfa drugs.
3) Amprolium (trade names include Coccivet):
 Amprolium is another anticoccidial remedy that can be used to treat coccidiosis in dogs and cats. As seen in the product image (right), it is also one of the more common medications used
to treat coccidiosis in birds.
Amprolium is another anticoccidial remedy that can be used to treat coccidiosis in dogs and cats. As seen in the product image (right), it is also one of the more common medications used
to treat coccidiosis in birds.
Dose rate: no greater than 300-400mg total dose orally per day (given once daily) for dogs [ref 2,23]. The drug is usually given for 7 days (can extend up to about 12 days) to dogs. The Veterinary Drug Handbook [Ref 30] suggests 100mg total dose once daily for 7-12 days in puppies.
Dose rate: no greater than 60-100mg total dose orally per day (given once daily) for cats [ref 2,23,30] .
Amprolium is generally administered for 5-7 days in a row [ref 1,2,23,30]. According to one reference (Nelson and Couto - 1), Amprolium can be associated with
toxicity in cats. Because of this, I would consider it a last choice option in this species.
Important note: Although this product (Amprolium) has been used successfully
in many dogs and cats with coccidiosis and is referenced in many top-quality veterinary textbooks, we must make you aware that this product is not currently registered for use in dogs and cats (i.e. it is being used off-label and in a way different to that for which it was designed). Consequently, your veterinarian, the drug company manufacturer and this website (us) can not
be held accountable should you decide to use this product in your feline or canine
companion and should you experience any adverse side effects with it.
Author's note: I have no personal experience with Amprolium in dogs and cats, only in
birds and poultry. I would personally avoid it in cats, due to the unknown toxicity features.
4) Toltrazuril (trade names include Baycox):
 Toltrazuril is another anticoccidial drug that is commonly be used to treat coccidiosis in dogs and cats. As seen in the product image (right), it is also one of the more common medicines used
to treat coccidiosis in piglets.
Toltrazuril is another anticoccidial drug that is commonly be used to treat coccidiosis in dogs and cats. As seen in the product image (right), it is also one of the more common medicines used
to treat coccidiosis in piglets.
The piglet preparation pictured on the right is the Toltrazuril product
that our clinic uses in coccidiosis-affected dogs and cats in our own clinic. Most of the clinics that I have worked in within Australia have stocked this product for the treatment of coccidiosis in dogs and cats - its use is widespread.
Dose rate: 15mg/kg (range 5-20mg/kg) orally, once a day (cat or dog)[ref 2,29]. A dose rate of 30mg/kg once daily for 3 days has been suggested for cats [ref 29].
Dose rate: the piglet suspension pictured is commonly given at 0.4ml/kg orally, once a day (cat or dog).
It is generally administered for 3-5 days in a row [ref 2].
It is available as a syrupy suspension for ease of administration.
There is also an injectable form of Toltrazuril available for animals who are not taking oral medications.
Important note: Although this product (Toltrazuril and Baycox Piglet) has been used successfully
in many dogs and cats with coccidiosis, we must make you aware that this product may not be currently registered for use in dogs and cats (i.e. it may be being used off-label and in a way different to that for which it was designed). Consequently, your veterinarian, drug company manufacturer and this website (us) can not
be held accountable should you decide to use this product in your feline or canine
companion and should you experience any adverse side effects with it.
Author's update 21/11/09: A recent conference attended by the author discussed the treatment of coccidiosis in dogs and cats in animal shelter situations. Toltrazuril (Baycox) was considered by most shelter vets in attendance to be a highly effective treatment for the control of coccidiosis. Not only does it seem to work, but it also comes as a liquid formula for easy dosing, it is palatable and it only needs to be given once a day for about 3-5 days.
5) Other drugs:
Other drugs, including Quinacrine, Spiramycin, Ponazuril and Roxithromycin have been trialled
in dogs and cats with coccidiosis with variable success. Ponazuril, a close relative
of Toltrazuril, may be of use in cats and horses afflicted with the neurological coccidial disease Sarcocystis neurona.
Some doses:
Ponazuril - 7.5-15mg/kg once daily for 1-3 days in dogs and cats. [ref 2,29]
Diclazuril - 25mg/kg once daily for a single dose in the cat. [ref 29]
Quinacrine - 10mg/kg once daily for 5 days in the cat. [ref 2,32] This drug is not longer available in many countries, including the USA.
Important note: It has been brought to the author's attention that some of our readers have been using this page to self-diagnose and self-treat coccidia problems in dogs and cats
without first seeking veterinary attention. PLEASE DO NOT DO THIS. Although this website makes every attempt to be accurate and up-to-date - recommended drug treatments, drug doses, drug durations and drug-safety recommendations change constantly and we may not always be able to keep up with the most-current knowledge. Some of the drugs listed on this page have important side effects and not all drugs and doses will be safe for all individuals (e.g. some dose rates may be toxic in some individuals). You must get your vet to diagnose coccidia in your pets (do not self diagnose) and recommend the best and safest treatments for your situation.
Please read our disclaimer. This website (us) is designed for information purposes only - so that you will know what options might be available to you and what questions and topics to ask your own vet about. It is not designed to replace your own vet's opinion. Your vet can directly examine your animal - we can not. This website will not be held accountable should you decide to use any listed product in your pet and should you experience any adverse side effects with it.
We have removed the dose rates for albendazole and fenbendazole out of a concern for our readers' pets. Despite our warning about the off-label nature of these two drugs; our disclaimer and our warnings about the risks of self diagnosis and the self-dosing of pets, people have been dosing their pets with these two drugs without direct veterinary advice and guidance. Neither drug is particularly good at treating coccidiosis compared to most of the other drugs mentioned, so their inclusion in the list is non-essential. The risks of their use far outweigh the benefits - hence we have removed them. Please be advised that all of these listed drugs (e.g. ponazuril, trimethoprim-sulfa, amprolium and so on) can have nasty side effects in certain individuals. Albendazole, in particular, can have very serious, even life-threatening side effects and should never be dosed without veterinary guidance.
Once again, please do not treat your own pets for any diseases without direct veterinary guidance. Only vets who have directly examined your pet can tell you which drugs and doses are most effective and safe for your animal. No website can guarantee this like your own clinician can.
Although some of these coccidial treatments are available as formulations for mixing into animal feeds
and water-sources, it is always best that you dose affected animals individually,
if possible. Sick animals are unlikely to drink or eat as well as healthy animals and might, therefore, miss out on their share of much needed antimicrobial drugs.
Some livestock feeds and preparations contain other coccidiostatic compounds such as
Monensin and Lasalocid and Decoquinate. These compounds should not be given to
cats or dogs. Monensin and Lasalocid are very toxic to horses and should never be fed
to this animal species.
7b) Antibiotics - drugs used to kill secondary bacteria.
The use of antibiotics in animals that are affected with clinical coccidiosis is variable
and varies from vet to vet and case to case. Some vets use them in addition to the coccidiostatic drugs and some vets do not.
As mentioned in section 4b, animals with coccidiosis suffer a lot of damage and inflammation to the
lining of their gastrointestinal tracts and are, therefore, at risk of developing severe secondary infections from bacteria present in the intestine and colon. If it is severe enough, this infection can potentially lead to bacterial infection of the blood and other organs, resulting in septic shock and even death for the patient. Antibiotic medications may be a valid form of additional treatment for these coccidia patients because they may prevent secondary bacterial infections from occurring.
Personally, I would always give antibiotics to coccidia patients that are very unwell;
that are febrile (feverish); that have a very high or low white blood cell count; that have toxic changes
in their white blood cells or that have a lot of blood in their faeces. Put it this way, if blood
can get from the blood vessels into the intestines (seen as blood in the poo), then bacteria
can surely get from the intestines into the blood. Patients that are very bright and alert
and well-looking might not need additional antibiotic cover, however, I would give them antibiotics if there was a lot of blood in the stools.
Commonly used antibiotics include:
1) Trimethoprim sulfonamide combinations (trade names include Tribrissen, Trivetrin):
 Again, the trimethoprim and sulfonamide (TRMS) combination drugs are an excellent choice in
these animal patients (provided these patients are not too dehydrated, debilitated, young or old). These drugs have the best effect against coccidia and they are highly effective at killing many of the secondary bacterial types that commonly complicate gastrointestinal infections, including: Streptococcus, Staphylococcus, E. coli, Klebsiella, Clostridium, Proteus and Salmonella. Using TRMS drugs in animals with coccidiosis is handy because it kills two birds
with one stone: TRMS takes care of both the primary coccidial organisms and the secondary
invaders, thereby avoiding the need for owners to give two separate types of antibiotics to
their canine and feline pets.
Again, the trimethoprim and sulfonamide (TRMS) combination drugs are an excellent choice in
these animal patients (provided these patients are not too dehydrated, debilitated, young or old). These drugs have the best effect against coccidia and they are highly effective at killing many of the secondary bacterial types that commonly complicate gastrointestinal infections, including: Streptococcus, Staphylococcus, E. coli, Klebsiella, Clostridium, Proteus and Salmonella. Using TRMS drugs in animals with coccidiosis is handy because it kills two birds
with one stone: TRMS takes care of both the primary coccidial organisms and the secondary
invaders, thereby avoiding the need for owners to give two separate types of antibiotics to
their canine and feline pets.
Additionally, the trimethoprim-sulfa drugs are particularly useful because they are able to access many tissues (including the brain). This makes them a potential future choice
for emerging protozoan brain infections such as Sarcocystis neurona.
Remember these cautions: trimethoprim/sulfonamide (TRMS) drugs should be avoided or used very cautiously in very young animals, very old animals, animals with kidney issues and in very dehydrated animals because they have the potential to cause renal problems (crystals of TRMS will deposit in the kidneys, leading to renal injury).
TRMS has the potential to cause dry-eye (keratoconjunctivitis sicca - KCS) in susceptible individuals
and caution should be exercised, particularly in KCS-prone breeds like cocker spaniels
and cavalier king Charles spaniels. Trimethoprim/sulfonamide combinations should be avoided
in certain breeds, especially the dobermann and weimeraner, because of the risk of drug
induced autoimmune joint disease and skin disease.
Dose rate: 15mg/kg orally, twice a day. It is generally administered for 10-14 days
when used in an antibacterial capacity (5-20 days for coccidia). Note that larger dose rates
are used when killing coccidia.
2) Clavulanic acid/amoxycillin combinations (tradenames include Augmentin, Clavulox, Noroclav):
Many of the bacterial infections that complicate simple cases of enteritis, colitis and coccidiosis are
quite responsive to the antibiotic, amoxycillin. Amoxycillin is a B-lactam antibiotic, closely
related to penicillin. Because some of the strains of Streptococcus and Staphylococcus
are now resistant to amoxycillin on its own (these bugs make penicillinase, an enzyme which destroys the drug), this antibiotic is generally combined with a secondary antibiotic called clavulanic acid, which helps to overcome this bacterial resistance (it inhibits penicillinase).
Amoxycillin is effective against a range of bacterial pathogens that commonly complicate enteritis and colitis, including: Streptococcus, Staphylococcus, Corynebacterium, E. coli, Klebsiella, Salmonella, Campylobacter, Clostridium and Proteus. Amoxycillin/clavulanic acid combinations are safe to use in most dogs and cats, including young puppies and kittens, pregnant and lactating bitches and queens and dehydrated or very sick animals.
Dose rate: 15-20mg/kg orally, twice a day. It is generally administered for 10-14 days.
Clavulox is also available as a syrup for easy administration.

Image - Clavulox can be used in animals with small and large intestinal diarrhea.
3) Enrofloxacin, orbifloxacin and other fluoroquinolones (trade names include Baytril and Orbax):
The fluoroquinolones are one of the newer antibiotic families to appear on the veterinary market.
These are great drugs with a good spectrum of action against many of the bacteria
that complicate coccidiosis, including: E. coli, Klebsiella, Clostridium, Proteus, Campylobacter, Yersinia and Salmonella. They even kill Pseudomonas. They tend
to be more expensive than many of the aforementioned antibiotics (especially in large dogs)
and, because of their relative 'newness', many vets choose to use them as a last resort (reserved for severe infections only) in order to limit the evolution of bacteria
that are resistant to them. Some bacteria are only susceptible to fluoroquinolones now
and we are trying to reduce the development of antibiotic resistance to these drugs by not overusing them.
Cautions: Fluoroquinolones are safe for most animals, however there are some side effects that
need to mentioned. These drugs should not be used in dogs under 12
months of age (under 18 months of age for large breeds) because of toxic effects that the drugs have on growing
bone cartilages. They should be avoided in cats of all ages, where possible, because of links with
sudden retinal atrophy and permanent blindness. Seizures and strange neurological signs
have been occasionally seen in animals subjected to high-level, prolonged dosing with fluoroquinolones. It is possible for fluoroquinolones to crystallize in the urine and to cause renal failure
(particularly if used at very high doses) and, therefore, these drugs should be used cautiously in very old animals, very debilitated animals and animals with pre-existing renal compromise.
Fluoroquinolones can potentially be associated with tummy upsets (inappetence, vomiting and diarrhea) and so owners need to watch out for
these signs and call their vet if they occur.
Dose rate: Baytril - 5mg/kg orally, once a day. It is generally administered for 10-14 days.
Baytril is available as a syrup for easy dosage.
Baytril can be given subcutaneously and even intravenously in sick or inappetent or vomiting animals.

Images of the fluoroquinolone drugs, Baytril and Orbax.
4) Metronidazole (trade names include Metrin, Metrogyl, Flagyl and Metronidazole):
Metronidazole is an antibiotic drug that is commonly given to animals with diarrhea
because it treats against a broad range of intestinal and colonic bacteria and protozoa, including Giardia, Clostridium, Campylobacter and other enterobacteria. It is
not particularly useful for treating coccidia-type protozoans, however, which is why it is included
in the antibacterial section and not in the anticoccidial section.
Metronidazole is also thought to have an anti-inflammatory effect on intestinal tissues and may go some way towards reducing the symptoms of inflammation and discomfort
seen in patients with severe enteritis and colitis.
Cautions: Metronidazole is safe for most animals, however there are some side effects that
need to mentioned. Seizures, vestibular disease symptoms and other strange neurological signs have been seen in animals subjected to high-dose-rate, prolonged dosing with metronidazole. These signs may be reversible if the drug is discontinued.
Metronidazole can potentially be associated with tummy upsets (inappetence, vomiting and diarrhea can result) and so owners need to watch out for
these signs and call their vet if they occur. The oral preparations of metronidazole taste particularly foul and can put some animals (particularly horses) off their food if given orally.
Dose rate: 15-25mg/kg, orally, twice daily. It is generally administered for 10-14 days.
Metronidazole is available as a syrup (Flagyl suspension) for easy dosage.
Metronidazole can also be administered intravenously or subcutaneously in sick or inappetent or vomiting animals.


Image 1: Metrogyl is one form of Metronidazole tablet available on the market for our furry friends.
Image 2: The intravenous Metronidazole BP preparation.
5) Doxycycline and other tetracycline drugs (trade names include Vibravet):
The tetracycline drugs, particularly doxycycline, are used in the treatment of a wide range of canine and
feline infectious disease conditions. They are effective against a very broad variety
of infectious disease organisms and their spectrum of action includes many of the organisms commonly implicated in gastrointestinal diseases. As an extra bonus, the tetracycline antibiotics are able to penetrate a wide range of tissue types and gain access to the inside of animal cells (which aids in the killing of hard-to-reach intracellular bacteria).
They are also thought to have an anti-inflammatory effect on intestinal tissues and this
may go some way towards reducing the symptoms of inflammation and discomfort experienced
by patients with enteritis and colitis.
Cautions: Tetracycline drugs are quite safe for most dogs and cats of any age, however there are some side effects that need to mentioned. Tetracycline drugs have the potential to cause browning of the developing permanent teeth of an animal, when given to animals under 4 months of age. For most owners, this staining will not be of concern, but owners of show animals might want to be mindful of the potential. Doxycycline can potentially be associated with stomach ulceration and tummy upsets (inappetence, vomiting and diarrhea can result) and so owners need to watch out for
these signs and contact their vet if they occur. It is sometimes possible for tetracyclines other than doxycycline to cause renal failure and, therefore, these drugs should be avoided in very old animals, very debilitated animals and animals with pre-existing renal compromise.
Dose rate doxycycline: 5mg/kg orally, twice a day. It is generally administered for 10-14 days.
Vibravet is available as a paste for easy administration.
Important: Doxycycline tablets should be washed down with water (via a syringe) after giving so
that they go all the way to the stomach and do not sit in the esophagus. This is important
because doxycycline tablets and capsules have been known to cause severe oesophageal ulcers
and strictures if they get stuck here.
Oral tetracycline drugs should not be given with food that contains calcium (e.g. milk, bones)
or magnesium or other cations because these reduce its absorption from the gut.

Images of VibraVet, a doxycycline formulation.
6) Other drugs:
Tylosin at 10-25mg/kg three times daily for 2-3 weeks has been found to be effective
in treating a range of colonic and enteric infections.
Chloramphenicol has also been used in treating colonic bacterial infections - it has severe human health implications (aplastic anaemia) and should be only used as very last resort.
7c) Intravenous Fluid Support.
1) Intravenous Fluids:
Kittens and puppies that develop severe coccidia-associated enteritis and colitis are at risk of temporarily losing one of the intestine's major functions: the absorption of water from the
intestinal tract. Not only are these animals unable to absorb the water that
they drink, they are also pouring massive amounts of inflammatory fluid, intestinal-secretory fluid and moisture-containing mucus out of the walls of their injured bowels, into their faeces. Severe, watery diarrhea results and these young animals will often dehydrate very quickly. Owners
will think their pup or kitten has suddenly lost weight, it has shrivelled away so
quickly from dehydration.
Often these animals are losing so much water from their intestines that they are completely
incapable of drinking enough water to keep up with the losses. Additionally, much of what
they are consuming, water-wise, is not being absorbed into the body anyway because their intestinal water absorption is so impaired. Much of the water ingested goes straight out the back end. Puppies and kittens with severe coccidiosis (especially patients with severe colitis) almost always need intravenous fluid support. It is the only way to get fluids into these animals when they are unable to properly absorb water from their intestines.
Author's note: sometimes, puppies and kittens come into the vet that are so collapsed and severely dehydrated (with severe shock signs), the veterinarian can't get an intravenous catheter into their leg veins. The blood vessels in their legs have shrivelled down to such tiny, thin tubes that no intravenous catheter will thread up them. In these cases,
the vet will sometimes be forced to put a catheter into the pet's jugular (the large vein in the neck) or insert a needle into the bone marrow of the animal's thigh (femur) or upper arm (humerus) to administer the fluids. Don't be alarmed to see your vet do this: it looks brutal, but these techniques are perfectly acceptable ways of giving lifesaving fluids to young animals in severe shock.
As mentioned in section 4b, often severe diarrhea is associated with a marked loss of blood salts (called electrolytes) into the intestines. These losses can be replaced by placing
electrolyte supplements into the intravenous fluids that are given to the young animal. Glucose levels can also become very low in puppies and kittens with severe gastroenteritis and
secondary bacterial infections (the body's glucose gets gobbled up by multiplying bacteria and by the inflammatory cells that come in to treat the disease) and so glucose may also need to be added to the intravenous fluids to keep the pet's blood glucose levels normal.

Pictures of intravenous fluids and the electrolyte supplements (potassium, phosphate etc.) used to correct electrolyte abnormalities in pets with enteritis and diarrhea.
2) Special intravenous fluids - colloids:
Puppies and kittens with severe ulceration and inflammation of the intestines can lose massive
amounts of inflammatory fluids and blood proteins out into their faeces (inflammatory fluids
contain large quantities of blood-derived proteins). Over a matter of days, these losses can accumulate, resulting in a massive drop in the animal's overall blood protein levels, a deficit that is further exacerbated should the animal go on to develop severe intestinal bleeding (blood contains lots of protein - intestinal and colonic bleeding can result in loads of blood protein pouring out of the pet's bowel, into its faeces).
When dogs and cats lose excessive amounts of protein into their intestines, their overall
blood protein levels can plummet. Of particular importance is a protein called albumin. Severe drops in blood albumin levels can have severe repercussions for the animal's health, body-functions and survival. Albumin has a large number of essential functions within the body,
one of the most important being the maintenance of colloid-oncotic pressure (COP). Colloid-oncotic pressure (COP) is a force that is exerted by the charged particles (e.g. blood salts) and heavy molecules (e.g. albumin) that drift in the bloodstream, which acts to keep
the watery fluid present in the blood (the plasma) within the blood vessels. Without this COP force, the blood's fluid will leak out of the blood vessels, resulting in a severe drop in the animal's
blood pressure (i.e. not enough blood for the organs) and infiltration of watery fluid into areas of the body where it is not wanted (e.g. the lung and the brain!)
When albumin is lost during severe coccidial infections, there is a risk of the animal's
colloid-oncotic pressure falling. Veterinarians treat this situation by either:
1) giving the patient special, synthetic, intravenous fluids, which contain heavy molecules that mimic the COP
effects of albumin (these special fluids are termed colloids) or
2) replacing the lost albumin with real albumin by giving the animal a plasma transfusion (see next point).
Colloids can also be given to puppies and kittens that come in to the vet clinic with severe signs of shock and low blood pressure, regardless of their blood protein levels. Because they act to increase the colloid oncotic pressure inside the animal's blood vessels, they can act to draw fluid into the blood vessels from other areas of the body, thereby boosting the animal's blood pressure rapidly whilst the animal is being properly and concurrently hydrated with other fluids.
Cautions: Colloids are great products, but they don't come without risks. They are artificial synthetic substances and, as
such, they have the potential to cause allergic and anaphylactic reactions in patients
given them. Colloids also have the potential to instigate bleeding problems in animals that have low blood platelet levels and they can sometimes cause an animal's blood pressure to become too high
(adding to bleeding risks).
3) Special intravenous fluids - plasma:
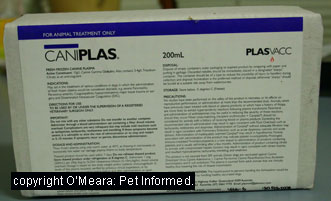 Plasma is the fluid that remains when you remove all of the cells from blood. It contains
several helpful substances that can really make a huge difference to the survival chances of coccidia puppies and kittens.
Plasma is the fluid that remains when you remove all of the cells from blood. It contains
several helpful substances that can really make a huge difference to the survival chances of coccidia puppies and kittens.
These include:
1) albumin - as mentioned before, albumin is responsible for maintaining colloid oncotic pressure within the bloodstream of puppies and kittens so that their blood vessels
don't start leaking. Albumin is also responsible for many other functions within
the body, including the transport of certain hormones, antibiotics and therapeutic drugs through
the bloodstream.
2) immune-modulatory proteins (e.g. some inflammatory proteins) - these assist the body
in generating an effective immune response.
3) proteins that mediate blood coagulation - many severely septic animals (e.g. animals with secondary bacterial invasion of the blood) develop
life-threatening disorders of their normal blood clotting mechanisms: a problem termed DIC (disseminated intravascular coagulopathy). In DIC, the patient's bloodclotting
mechanisms are disrupted: the blood either wants to clot excessively, leading to blood-clots, embolisms and 'strokes' or, alternatively, it does not want to clot at all, leading to excessive bleeding. Plasma contains the necessary blood-clotting regulatory compounds required to treat this critical complication.
Plasma is more expensive than the synthetic colloids are, however, it contains many helpful elements in it that the synthetic colloids do not. Plasma is the only source of
'true' albumin replacement for an animal that vets can give. Although the synthetic colloids
do do a good job of replacing COP, they can not replace the many other functions that
only 'true albumin' can do (e.g. drug transport).
Author's note: a lot of plasma (many bags of it) needs to be given to a large dog
to generate any noticeable shift in its overall protein and albumin levels. This can get
expensive. Fortunately, most of our severe coccidia patients are young and small (under 4kg)
and, therefore, smaller quantities of plasma are able to make a bigger, more noticeable
difference, in their protein levels, thus reducing the costs of treatment.
Cautions: Also note that plasma, like the synthetic colloids, is not without risk. It is a
proteinaceous substance being given intravenously. Consequently, there is the possibility that a plasma transfusion could cause allergic or anaphylactic reactions in some patients,
particularly if the patient in question has received plasma, blood or tick or snakebite antiserum
previously.
7d) Special intravenous fluids - blood:
 Some patients lose so much blood as a result of gastrointestinal and colonic ulceration that they
can actually become severely anemic in addition to losing protein into the gut.
Some patients lose so much blood as a result of gastrointestinal and colonic ulceration that they
can actually become severely anemic in addition to losing protein into the gut.
These patients may require a blood transfusion (containing red blood cells)
to replace those red blood cells lost into the gut and faeces. If whole, fresh blood
is available (blood taken freshly from a donor within the last few hours), this can be particularly helpful to the patient. In addition to red blood cells, freshly-drawn, whole blood contains much-needed albumin, plasma antibodies and also live white blood cells. Septicaemic dogs and cats often have low white blood cell counts (the cells are lost fighting
the overwhelming infection) and, consequently, live white blood cells in a blood
transfusion may be of some help in fighting the infection.
Caution: Please note that blood transfusions, like synthetic colloids and plasma, are not without risk. Blood is a proteinaceous substance being given intravenously. Consequently, there is the possibility that a blood transfusion could cause severe (even fatal) allergic or anaphylactic reactions in some patients (particularly cats), particularly if that animal
in question has received plasma, blood or tick or snakebite antiserum previously.
Generally, most dogs can receive a first blood transfusion from any canine donor without
the need for cross-matching of blood. Subsequent transfusions can also be given
without cross-matching, if they are given within 48 hours of the first one. Cross-matching is required for any blood transfusion given 48 hours or more after the first transfusion.
Cats must be blood typed before any blood transfusion, even the first one. Cats have very specific
blood types (A and B and AB) and must only receive blood of the correct type. In an emergency (i.e. if a cat donor can not be found), a one-off transfusion of canine
blood can be given to a cat.
7e) Diet Management.
Animals that present to the veterinarian with symptoms of coccidial enteritis can often benefit
from a diet that is bland (won't disturb the gut) and easy to digest. Diets based on
bland, skinless, non-fatty, white meats such as rabbit, chicken or turkey (not fish) and bland carbohydrates
such as rice and potato (rice is better) are ideal for the damaged gut.
There are many excellent, fully balanced, veterinary prescription diets available these days, which be given to animals of all ages that are convalescing from any form of intestinal upset. These include, Hills Science Diet i/d (cat and dog forms) and Royal Canin Digestive Diet. Alternatively, you can feed your recuperating pet on boiled, skin-free chicken
breast and well-rinsed rice (rinsing the rice thoroughly after cooking to remove the starch)
for a week, while its intestines and colon settle down and heal. This home-made diet is not
balanced and not appropriate for long-term feeding, but it is fine to give for a week or so.
Some animals will refuse to eat the bland prescription diets but will happily tuck into home-cooked chicken and rice - it just gives you another option.
Whatever food you choose to give, should be given little and often. Animals
with sick intestines should only be fed small quantities of food
(e.g. 1-2 tablespoons) at a time and these amounts should be given frequently - every couple of hours. Large quantities of food entering the injured intestine are more likely to be vomited up or go through the damaged gut undigested and wasted. Smaller quantities are tolerated
much better. Give the food every few hours so that the pet is getting its daily nutritional
requirements.
Food can be made more palatable by heating it in the microwave. Don't make it too
hot!
Avoid fatty foods when the intestine is injured!
Animals that are vomiting up food will often benefit if they are fasted for 24-48 hours. This rests the intestinal tract and allows it to heal a bit before more food is given. Water should not be withheld.
Animals that are in hospital with severe gastrointestinal signs, anorexia and diarrhea can be
given assisted feeding, either by nasogastric tube (a tube placed from the nose into the stomach)
or esophageal-gastric tube (a tube placed from the oesophagus into the stomach). A PEG
tube (tube going directly into the stomach) is seldom required.
Intravenous nutrition can be given to animals that are unable to keep down any oral foods or absorb any foods from their intestines. This would seldom be required for most cases of coccidiosis.

8) What is the prognosis for coccidiosis in dogs and cats?
Most cases of clinical intestinal coccidiosis that present to the vet and are treated with appropriate
antimicrobial therapies do very well. As a general rule, the prognosis for clinical recovery from non-complicated cases of coccidia infection is excellent. It must be mentioned, however, that, because many of these successfully-treated animals do go on to develop a persistent, non-clinical,
carrier state (i.e. they retain live coccidia organisms in their colons), the prognosis
for complete coccidial clearance is moderate to poor. Put simply, the prognosis for
recovery and resolution of clinical signs is excellent, but the prognosis
for clearing the organisms completely from the body is poor.
Very young, malnourished and undergrown animals that present with severe signs of coccidiosis
must be considered to have a more guarded prognosis. These animals often have very little
nutritional and immune system reserves to fall back on when they become ill and they are more
likely to succumb to secondary complications such as lack of blood sugar, secondary bacterial
infections and low blood proteins. Surgical complications such as intussusception and
rectal prolapse seem to be more common in very young animals too.
Young animals with concurrent intestinal diseases such as intestinal worms, Clostridium
infection and Campylobacter infection should also be considered to have a poorer
prognosis.
Older animals that develop recurrent or long-term (chronic) coccidial infestations
should also be considered to have a guarded prognosis too. It is not common for clinical signs of coccidiosis to persist in older animals and such animals should be suspected
of having some form of underlying intestinal disease or immune disorder. Failure to
treat the underlying causes will result in a failure to clear the clinical signs of
coccidiosis for any long-term period.
The prognosis for Sarcocystis neurona in cats (and horses) is very guarded.

9) How to prevent coccidia in puppies and kittens and adult pets.
Currently, there are no vaccines available for the prevention of coccidia in puppies
and kittens. As a result, prevention of coccidiosis involves reducing your pet's chances of coming into
contact with contaminated environments and faeces and enhancing the health, body condition and immunity of your animal.
9a) Avoid contact with infected dogs and cats and contaminated environments:
Because most cases of coccidiosis occur when puppies and kittens are exposed to stressful environments
that contain lots of dogs or cats all co-existing in close proximity to each other, it stands to reason that coccidiosis can often be prevented by not placing your pet in these situations. Boarding your dog or cat with friends or getting a house-sitter to look after your house and pet while you go on holidays can be a low-disease-risk alternative to boarding your dog or cat in a boarding kennel or cattery. Making sure that your fences and yard are dog-proof and keeping your cat indoors (or in a special
cat aviary) can reduce the risk of your friend getting out and ending up in a pound or shelter where
coccidiosis is rife.
Sometimes, of course, you do have to place your pet in environments where there are
many other dogs and cats and thus the potential for parasitic disease spread. There are precautions that you can take, however, to reduce this risk. Some handy tips include:
1) Vaccinate your pet within 6 months of attending a show event or boarding kennel/cattery:
Although vaccines do not protect your pet against coccidia, it is important that
your pets are protected against vaccinatable diseases when they go to kennels and
catteries. Animals need a strong immune system to fight off and prevent coccidiosis
and making sure that your pet does not contract some other preventable disease
(e.g. parvo, kennel cough) can help to keep your pet's immune system strong. Animals
that become sick as a result of parvovirus or other vaccinatable diseases become
stressed. This stress of illness suppresses their immune systems (and, in the case of parvo, damages their intestines), making it easier for coccidia to get a foothold.
Vaccine-induced immunity is strongest within the first 6 months of a vaccine and, therefore, vaccinating your dog a month or two before it meets other pets will reduce its risk
of contracting a vaccinatable infectious disease.
2) Check out the boarding kennels or cattery for yourself before putting your pet in there:
Ensure that your pet's accommodation is suitable. Look for signs of poor husbandry and unsanitary conditions
that might promote disease spread. Does the place smell OK? Is the place well-cleaned
(look for excessive dustiness and dirt and faecal contamination). Are faeces
able to travel from one cage to another under doors and walls? Is the place well-ventilated or is it musty and enclosed with stale-smelling air? Are dogs or cats placed in yards together (which could enhance disease spread)? Do the animals share food and water bowls? Are the food and water bowls clean? Is the place overcrowded with animals? Are animals placed
in situations where they may become stressed (e.g. dogs and cats facing off against each other
through wire fences, cats all placed in together, extremes of heat and cold, inability to get dry, draughts etc.)? Look at the other pets in the place (if you are permitted to) - do you notice any coughing or sneezing animals or animals with watery or
loose stools? If you see any major problems, don't board your pet there.
3) Only attend boarding kennels, groomers and dog clubs which have strict vaccine requirements:
If they are being strict on you with your pet's vaccinations, you can be sure
that they are being strict on everyone else too. This strictness keeps disease out of a place. Lax rules result in diseases. Generally places with strict vaccine requirements
often have high standards of hygiene and cleanliness within the facility too - this
is vital to keeping coccidiosis under control.
4) Don't board young puppies and kittens:
Young pups and kittens are the most prone to contracting clinical signs of coccidiosis
and becoming very unwell. As hygienic as they try to be, kennels and catteries are often
overrun with adult animals that are non-clinical carriers of feline and canine coccidia. The faeces of these affected animals
can infect your young animal, making it very unwell.
5) Take your own food and water bowls to the boarding kennel, cattery or any dog shows or dog club events: This way your pet will not have to use another, possibly fecally contaminated, bowl.
When walking your pet, make sure that you keep him or her on a lead. This way, you will
be able to prevent your pet from running off and consuming the faeces of other animals. Never let your pet eat the droppings of other animals - poo contains lots of nasty
organisms that your pet might catch.
Similarly, do not let your pet hunt rodents or other animals and consume the uncooked meat or
offal from deceased animals. If you do like to feed your animal raw meat (especially
raw bones - after all, bones should never be fed cooked), then make sure to freeze the meat for a minimum
of 3 weeks before feeding it to your animal. This will kill any infectious coccidian tissue
cysts. I do not advise feeding raw offal to dogs at any time (because of the risk of hydatid
tapeworms), however, well-cooked offal (lung, liver, heart etc.) is fine.
When purchasing a pet for the first time, consider where your pet comes from. As mentioned
in section 3, there are certain environments and facilities that are more likely to have high levels of
coccidiosis and, thus, are more likely to sell you a coccidia-affected puppy or kitten. Petshops, shelters, pounds and poor-quality dog and cat breeders are more likely
to have coccidia on their premises. Make sure that, if you do buy a puppy or kitten from
one of these places (or any place, really), the kitten or puppy is well-grown (not stunted) and
of good bodyweight and condition (a nice shiny coat and a bright, alert and interactive behavior). Do not buy sickly, lethargic, sleepy puppies and kittens, nor any that are underweight
or which have poor coats or pot-bellies. Also make sure that any purchase comes with, at minimum, a 2 week wellness guarantee. It is not uncommon for puppies and kittens to seem fine in
the store and then break out with coccidia a few days after you bring them home because
of the stress of moving-house.
Obviously, I do not want to put you off buying a pound or shelter animal - these animals
often make great pets and are sorely in need of a loving forever home. Just make sure that
the animal (dog or cat) is placed on a course of coccidial treatment (even if it not
symptomatic for the disease) prior to you taking it home. Also, make sure that the animal is well-vaccinated
and wormed prior to you taking it (remember that other intestinal diseases and parasites can make
coccidiosis worse).
Be aware of the potential for you or other people or animals to bring disease home to your pet. If you have visited a place where there has been coccidia infection (or any outbreak of infectious disease, for that matter), don't bring the disease back to your house on your hands or clothes, where your pet can catch it! Change your clothes, disinfect your shoes and shower thoroughly (this includes washing your hair)
before greeting your pet. Ideally, disinfection should take place somewhere other than
your own home. The same precautions should also be taken when other people visit your home:
ask them if they have had any potential contact with infectious animals, puppies and
kittens with diarrhea etc.
If you have had a case of coccidiosis in your own home and/or yard previously, then you will need
to disinfect any contaminated areas and feed bowls in order to make them safe for any new puppies
and kittens that you bring home in the future (see section 11 below on coccidia decontamination). Coccidial organisms are resistant to many kinds of physical and chemical disinfection techniques and thorough cleaning is required to remove the organisms.
9b) Enhancing the health, body condition and immunity of the animal.
A big part of infectious disease prevention, particularly clinical coccidial disease prevention, requires the activity of a healthy, fully-functioning immune system. Although avoidance
of the infectious organisms (avoiding faecal-oral transmission and ingestion of infected
tissues and organs) is key to preventing the disease, the overall health and wellbeing of the animal is critical if there is to be a strong immune system
response towards the parasite, should your animal ingest it. Disease prevention involves a holistic approach, with nutrition, exercise and mental health care all important parts of the process. Animals that are in good body condition and which have been given a balanced diet and are well-exercised and emotionally sound (e.g. not overly stressed or bored etc.) will generally be more resistant to disease and able to mount a better immune response.
Well-kept animals should not develop severe signs of coccidiosis (if any) and any period of
illness should be milder and more short-lived than that seen in poorly-cared-for pets.
Puppies and kittens that are malnourished and/or which harbour other bacterial and parasitic infections
in their intestines are more prone to severe coccidial infections. Thus, good
nutrition and control of intestinal parasites (worming etc.) is important in preventing and reducing coccidian severity.
Some hints and tips:
- Puppies and kittens and adult dogs and cats should be routinely wormed.
- Puppies and kittens and adult dogs and cats should be fed a completely balanced (AAFCO approved) diet.
- Puppies and kittens should be played with often and exercised within the home until fully vaccinated
(this human contact fulfills their exercise and mental health needs, but keeps them safe
from disease until fully vaccine protected).
- Dogs should be walked twice daily (once vaccinated) for a bare minimum of 15-30 minutes at a time
to aid both their mental health (reduces boredom) and exercise needs. Cats can be walked, but
providing them with an outdoor playpen (e.g. large cat aviary) can be enough to provide
them with adequate exercise.
- Dogs and cats should have toys and adequate room to move (e.g. yard size, cat aviary) to reduce boredom and stress
whilst you are at work.
- Dogs and cats should not be overfed or allowed to become obese.
- Dogs and cats should not be kept in dusty, irritant or poorly-ventilated air conditions.
- Dogs and cats should be kept in low-stress, dry, clean, sanitary environments with no extremes
of heat and cold, no draughts, good shelter and no build-up of urine or feces.
- Any known stressors should be identified and removed, if possible.
- Purchasing in-bred animals should be avoided - excessive in breeding may result in appearance of genetic immune disorders.

10. Controlling feline and canine coccidia in high-risk and/or already contaminated environments.
The following discussion mostly revolves around the control and management of Isospora - coccidia
species that are transmitted from dog to dog and cat to cat through the fecal oral route of
transmission. The control of other coccidian species (ones that require a dog or cat to ingest
an intermediate host animal) is much simpler. These coccidian species can be simply controlled
by feeding cats and dogs good quality commercial diets and well-cooked meat or offal
and by preventing these animals from hunting live prey (rodent control is essential here) and scavenging for carrion.
Feline and canine coccidia outbreaks are quite common in large multiple-dog and multiple-cat facilities such as breeding facilities, shelters, pounds and even boarding kennels. Such
outbreaks and endemic infestations in a premises can become highly costly in terms
of treatment and isolation (staff care) of sickly animals; disinfection of infected
premises; lost reputation and lost productivity (sickly, stunted puppies and kittens that can't be sold
and reduced fertility of unwell breeding animals). Consequently, large dog and cat facilities need to have protocols in place that will help them to prevent coccidia and help them to deal with an outbreak of coccidiosis, should it occur. Control and prevention of disease in these situations involves:
a) protecting the susceptible animals and preventing them from becoming infected,
b) reducing environmental parasite oocyst contamination and destroying the infectious particles and
c) reducing the non-infectious environmental and stress factors that can contribute to the disease.
10a: Protecting the susceptible animals.
In a situation of high coccidia risk or pre-existing contamination of the environment
with infectious particles, any very young or very old animals; any unwell animals (animals with pre-existing disease); any stressed animals (e.g. pregnant, weaning, growing or lactating animals) and any animals of high-risk, immunocompromised breed-lines are going to potentially be susceptible to infection. The risk of these animals, and any other dogs and cats in the facility, contracting coccidia can be reduced
in the following ways (this is by all means not an exhaustive list):
1) Ensure that all animals within the facility and all
those entering the facility are up to date with their vaccines.
Preventing animals from catching common, vaccine-preventable diseases can go some
way towards keeping an animal's immune system strong. Animals
that become sick as a result of parvovirus or other vaccinatable diseases become
stressed. This stress of illness suppresses their immune systems (and, in the case of parvo, damages their intestines), making it easier for coccidia to get a foothold.
2) Isolate pregnant bitches or queens and their litters from the rest of the dog and cat population.
Pregnant and lactating bitches are under massive levels of physiological stress and are, therefore, highly susceptible
to parasitic infections. Likewise, newborn puppies and kittens are also at risk of infection because their immune systems are not yet fully developed. Isolate bitches and queens
and their litters in easy-to-disinfect (e.g. tiled or concrete areas, not grass or soil) pens,
which have, preferably, never before been contaminated with coccidia*, from the time of whelping
(queening) to the time of weaning. These pens should be located as far away as possible from the main dog population so that fecal run-off does not contaminate the bitch's/queen's quarters. If whelping bitches and queens can be removed to a new non-contaminated premises altogether, while
decontamination of the coccidia-infected facilities is occurring, so much the better. All bedding and feed and water bowls provided should be new (or well-disinfected) and should be strongly disinfected or discarded after use by the bitch or queen. Steel bowls are
easier to disinfect (they can be autoclaved and boiled).
* Because of the high prevalence of non-clinical coccidia carriers, it can be very difficult
to tell whether an area has ever been contaminated or not.
3) Pre-emptively treat bitches and queens with coccidiocides.
Pregnant bitches and queens (pregnant cats) can be treated with coccidiostatic drugs
in the weeks just prior to whelping or shortly after whelping. This will greatly suppress
and reduce the numbers of oocysts being shed by carrier mothers and thus reduce the risk of coccidiosis affecting
the highly-susceptible newborn litters.
4) Ensure that puppies and kittens get their colostrum on time (<24 hours after birth).
Puppies and kittens must be monitored to ensure that they do get their colostrum (maternal immunity).
Bitches and queens that are recovering from caesarean section (unable to fed the young yet) or that are
initially reluctant to feed their offspring for other reasons can be milked of their colostrum
and this can be fed to the pups and kittens through bottle or stomach tubing.
5) Don't expose puppies and kittens to contaminated environments.
Puppies and kittens should, ideally, go from the safe whelping zones straight to their new owners.
The aim is to sell and get the young animals out of the infected environment ASAP. They should not come into close contact with the general canine and feline population, where coccidia shedders
are highly prevalent, nor should they come into contact with another animal's food or water bowls (which could be infected) or feces or any areas of the premises that are impossible to disinfect (lawns and soil). In extremely high-risk situations, early weaning (4-5 weeks instead of 6+ weeks) may be a consideration - try to get the pups and kittens out of the environment as early as possible.
6) Wear gloves.
Whelping bitches and queens and newborn puppies and kittens and other animals in high risk situations
should be handled with gloves (plastic disposable aprons are also available for the extra-cautious to shield dogs and cats from possibly-contaminated clothing). New gloves and aprons should be used for every litter to avoid passing infectious organisms from one bitch/queen (and litter) to the next. If possible, gloves should be used when handling all other dogs and cats on the premises too (though, cost-wise this might not be practical in a big population).
At a bare minimum, hands should be washed thoroughly after handling each dog or cat, prior to
handling the next.
7) Avoid in-breeding - i.e. don't breed susceptible animals.
In-breeding (e.g. breeding facilities) should be avoided to reduce the risk of genetic immune system disorders appearing and enhanced susceptibility to parasitic, viral and bacterial infections.
8) Control other easily-prevented diseases that might compromise an animal's gastrointestinal tract or immune system and make that animal susceptible to coccidial infection.
Gastrointestinal diseases (e.g. bacterial infections - Campylobacter and Salmonella) and high intestinal parasite burdens compromise the defensive mechanisms of the gastrointestinal system, reducing the ability of the bowel to clear coccidia and other
such parasites. Additionally, low-grade, chronic diseases (including parasitism) can cause chronic, low-grade stress, which may suppress the immune system's response to coccidia. Consequently, control of these other parasites and diseases, through appropriate medications and parasite programs (routine worming etc.), is essential.
Good hygiene is crucial here too: ensuring that all runs, feed bowls and water dishes are cleaned promptly of fecal and respiratory tract secretions and ensuring that excrement and secretions are not permitted to spread to other runs or kennels through gutters and run-off. Most
intestinal parasites and bacterial and viral infections are spread through fecal-oral routes: less fecal contamination; fresh, clean bowls; regular cleaning of runs and cages and
minimal fecal run-off between cages and runs (decent isolation of animals) means less disease transmission from animal to animal.
9) Avoid overcrowding of animals.
Overcrowding promotes rapid infectious disease spread from animal to animal; it
promotes stress which suppresses the immune responses of susceptible animals and overcrowding makes it
difficult for facility operators to identify the sick and to find a place, sufficiently out of the way, to isolate the sick, once they have been identified. With diseases like coccidiosis, overcrowding is of particular concern because faeces
are more likely to missed by cleaners (not seen) and stood in or consumed by other animals.
10) Don't keep young animals in places with adult animals.
Adult animals often carry coccidia: they shed the infectious oocysts in their faeces, which can then be ingested by susceptible younger animals. Similarly, do not mix younger animals
of different ages or sizes in the one pen.
11) Consider placement of food and water bowls.
Feed and water bowls that become contaminated with faeces as a result of puppies and
kittens walking through them (after walking through their own faeces), are an excellent
source of coccidia transmission from animal to animal. The animals can't avoid eating infected faeces if they are eating and drinking from infected food and water dishes.
Contamination of food and water dishes can be reduced by elevating the dishes off the ground a bit
(pups and kittens are more likely to walk around them then) and by placing the food and water dishes
at the back of the run, away from the action. Pups and kittens always rush to the front of a cage
in excitement when they see people and other animals - if the bowls are placed at the front of the
pen, they will be stepped in during the mad scramble. If the bowls are placed at the back of the cage, the young animals will be running away from them - they will be less likely to be trodden in. Frequent
cleaning and disinfection of food and water bowls is also important in coccidia control.
12) Reduce stress.
The number of susceptible animals is reduced when stress is low. This is discussed
in section 10C - reducing the non-infectious, environmental and stress factors that can contribute to disease.
10b: Reducing environmental contamination with coccidia:
In any place where coccidia has appeared, it is important to ensure that contamination is minimized
where possible (e.g. reduce the number of infectious particles that enter a 'contaminated' area); that the oocysts
are destroyed as thoroughly as possible (decontamination of the environment) and to ensure
that the infectious disease organisms do not spread from the contaminated regions to 'clean' regions of the premises and beyond.
1) Isolate infected or sick animals.
Because of the high prevalence of non-clinical coccidia shedders in the population, it can be
very difficult to completely remove coccidia-shedding animals from the general
animal population. In the presence of coccidia carriers, there will always be some level
of oocyst contamination of the environment.
Sick animals, however, with clinically obvious
disease signs of coccidia, do, as a general rule, tend to shed greater numbers of oocysts in their
faeces than non-clinical carrier animals do. The fact that these animals are displaying disease
signs suggests that the level of coccidia replication and oocyst production is greater
in these animals than in the carriers. Consequently, removing obviously sick animals
from the general animal population will go some way towards reducing the overall degree
of coccidial contamination of the environment.
Sick animals should be removed from the general population and put into a quarantine region well away from the other, unaffected animals. Typically, severely affected pets will go to the vet and the vet will isolate them in a special 'iso' - isolation - ward. This quarantine region should not be near any thoroughfares (places where animals and people frequently walk) and well out of the way.
Animals in quarantine should be handled as little as possible (though not infrequently enough
that they aren't getting proper care). When handled, the carer should wear disposable
gloves and a disposable gown. All materials used by the carer should be disposed of in bins present within the iso ward, so that nothing that is potentially fecally contaminated and
infectious gets brought out into the 'clean' areas of the premises. Shoes are generally washed thoroughly in disinfectant foot baths (see section 11) as the carer leaves the isolation area, however, disposable shoe covers (covers worn over the shoes in the isolation area) can be used as an alternative.
2) Quarantine areas where sick animals have been.
Areas where sick animals have been should be quarantined from other animals until thoroughly disinfected (see section 11) and rested. Coccidia are quite resistant
to a range of disinfectants and environmental conditions and so disinfection needs
to be very thorough.
3) Discard contaminated bedding.
Any towels or bedding that the sick animal has been in contact with should be discarded as garbage once soiled. In the case of coccidiosis, you could disinfect and salvage the
bedding if you really need it (e.g. if the bedding is really expensive or valuable), however, the best option is always to throw out contaminated items that
could harbour potentially infectious, parasitic particles.
4) Be mindful of run-off.
Be careful that run-off from quarantined areas does not travel to 'clean' areas
of the premises. Be mindful of gutters, gaps under the walls of pens and gaps in the walls of pens (e.g. wire fencing), that might allow fecal and diarrhea fluids from infected animals to contaminate clean areas or waterways. Be also aware of the 'sloping' of concrete or tiled
runs: ensure that liquid run-off from one pen can not run down a slope and into another.
5) All infected rooms, pens and fomites (feeding dishes, grooming gear, benches etc.) should be disinfected thoroughly before exposing other animals
to them.
6) Avoid overcrowding of animals.
Overcrowding promotes rapid infectious disease spread from animal to animal; it
promotes stress which suppresses the immune response and overcrowding makes it
difficult for facility operators to find a place, sufficiently out of the way, to isolate the sick.
7) Consider your choice of surfaces: you want surfaces
that don't hold or protect bugs and which are easy to clean and disinfect.
It is almost impossible to keep infectious diseases and parasites out of dirt flooring and
grassy areas: such surfaces are difficult to decontaminate and they tend to pool water, which promotes the growth or survival of infectious organisms. In the case of coccidia, surface choice is very important. You can not easily get at dirt or grassy areas of a yard with disinfectants and, because coccidial oocysts are somewhat resistant to heat, sunlight,
freezing conditions and drying conditions (desiccation), the oocysts will remain infective
to other animals for many months in soil and lawn.
Author's note: Coccidian oocysts do eventually die from sunlight, heat and desiccation, but
this can take weeks to months. Oocysts (the infectious stages shed in the poo) will survive freezing environmental temperatures for very long periods, even though the infective cysts found in the meat and offal of intermediate hosts do not.
It is far quicker and easier to rid your premises of coccidia (or at least reduce coccidial contamination)
if you can thoroughly disinfect your premises from top to tail. For ease of disinfection (including parvo etc.), you are better to go with cement or tile flooring, which can be easily cleaned of feces, urine, vomit and respiratory secretions and readily disinfected.
Choice of fencing/walls is important too. Smooth-textured (e.g. steel), solid, filled in walls
are easier to clean than wires or rough brickwork (which have a hugely increased surface
area for parasites, bacteria and viruses and feces to cling to). Solid, filled in walls also promote less
aerosol and faecal transmission of disease from dog to dog or cat to cat than open wiring does.
8) Routine cleaning is a must.
Routine sanitation and cleaning is a must in all dog and cat facilities. All surfaces should be routinely disinfected and kept clean. Feces and urine must be removed daily to twice daily
at a bare minimum. Routine spraying of runs with water to remove particulate matter and dust is important (these harbour infectious organisms and bacteria) and
intermittent (weekly to 2-weekly) steam-cleaning of surfaces is useful to reduce infectious
disease loads (even parvo is killed by steam-cleaning).
Don't forget to clean cage or door bars and vertical walls where an animal might have
smeared faeces.
9) New animals to a premises should be quarantined and given coccidiostats.
As a routine part of infectious disease prevention, all new dogs and cats to a breeding facility
or pound, shelter or boarding kennel should be quarantined away from the main dog or cat population for at least a month. The animals should be fully wormed and vaccinated and monitored for disease appearance. Only when the time of quarantine is up and the animal considered free from disease, should he or she be allowed into the greater animal population. Most animals with
coccidiosis should manifest obvious disease symptoms within this month, due to the stresses
associated with their relocation.
Note that this quarantine zone should not be an area that has had diseased animals
in it before, if possible. If the quarantine zone has had diseased animals in it previously, then it should have at least been thoroughly disinfected and spelled prior to the arrival of the new animal for quarantine. If not, the new non-diseased pet could contract diseases from the quarantine area.
Quarantined animals should be treated like isolation animals, with gloves, gowns
and foot bathing (or shoe covers etc) used to prevent disease going from the
quarantine zone into the rest of the population or from the rest of the population into the quarantine zone.
Animals newly admitted to a premises are usually vaccinated and wormed pre-emptively, however, they can also be treated with a coccidiostat too. Most anti-coccidial drugs are quite
safe and cheap to use and can be given to puppies and kittens and new arrivals in the absence of any
clinical symptoms. A lot of shelters routinely treat their new kitten and puppy arrivals
with coccidiostats in order to keep coccidiosis to a minimum.
In theory, households looking to introduce new animals into their already existent pet family could also employ a similar quarantine procedure. If this is not
possible or practical, new additions to the family should ideally be bought from reputable breeders or families (places with excellent standards
of pet care and hygiene) and vaccinated and wormed and given a coccidiocide (e.g. Baycox for three days)
prior to arrival.
10) Staff should know the signs of unwellness and coccidia infection in puppies and kittens.
Early detection of illness is key to establishing rapid isolation of an animal
and reducing the spread of diseases like coccidia. Staff should look out for lethargic, inappetent (or reduced appetite puppies) or 'loner' (puppies on their own) puppies and kittens. Puppies and kitties with any diarrhea, blood in the stools or excessively smelly or mucoid droppings should be immediately isolated and treated. Recognition of puppies in poor condition or unwell condition is very important in places like pet shops that receive lots of unvaccinated and unwormed puppies through their doors. These places should not take on any weak or sickly puppies to sell, as they risk contaminating their facilities and all the other healthy pups that
they get in.
11) Good record keeping.
Breeders that receive dogs and cats from elsewhere and pet shops that receive lots of for-sale
puppies and kitties from various sources must keep good records of where these animals have come from. Good record keeping allows these facilities to recognise breeders and sellers that
are frequent offenders and who frequently sell underweight, malnourished, wormy or coccidia-affected animals. Once identified, not buying from such places can go a big way towards preventing coccidiosis and other contagions from
getting into your facilities.
Good record keeping is also essential within large facilities such as pounds, shelters
and breeding kennels and catteries. Noting which runs and groups of cages tend to
get the highest numbers of coccidia infected animals can be very valuable. If certain
cages and dog runs tend to be frequent offenders, this lets operators know that there
is a problem to be solved in that area. Is the staff member responsible for cleaning
the cages not doing his/her job? Is the cage excessively draughty and cold and stressful? Does the run slope oddly, allowing for fecal spread and contamination? Is there a significant
insect or rodent source of infection? Does water tend to pool in those runs?
12) Control rodents and insects.
Rodents and insects can potentially carry coccidia organisms on their feet from animal to animal and place to place. Flies are a particular problem because they
are attracted to faeces and flit from dropping to dropping and cage to cage.
Strict control of these vectors must be put into place in order to reduce the spread of coccidia in a facility. Obviously, removal of factors which attract rodents (such as grass, grain, open dog-food packs and warm, hidden areas to breed) and flies (feces, open foodstuffs) is vital, but adequate control may need to include the use of rodent poisons and insecticides and 'fly traps'.
10c: Reduce the non-infectious, environmental and stress factors that can contribute to coccidiosis.
Stress lowers the immune system defenses of animals, making them more susceptible to showing disease
symptoms. Each point below addresses a different factor in stress-management:
Ensure that all animals have adequate nutrition. Happy, well-nourished
animals of good bodyweight generally have a better immune system and are better equipped to cope with disease.
Remember to treat each animal as an individual: regularly record the weight and body condition
of each puppy or kitten to ensure that the nutrition provided is adequate for him or her and
to ensure that the animal is actually getting fed. It is easy in crowded situations
for individual animals to be underfed (as an individual, they might simply need more food than is on offer) or for carers not to realise that a puppy or kitten is being bullied out of a meal. Remember
that nutritional monitoring is particularly important in animals that have high
metabolic requirements: pregnant dogs and cats, lactating dogs and cats, growing pups and kits and performance
animals (e.g. working dogs, sporting dogs and obedience dogs).
Temperature and moisture control. Making sure that kennels, cages and runs are warm and dry and free of draughts and chills
will also go a ways towards keeping animals comfortable and stress-free. Temperature control
in runs is important: excessively cold and hot conditions are stressful and can facilitate disease. Constantly fluctuating temperatures are also stressful, even if the swings are not extreme: maintaining a steady-state, comfortable temperature
is ideal. According to Greene CE, temperatures in kennels should be between 21-24 degrees-C. Remember that temperature control is particularly important in animals that have other stresses (you don't want to add temperature issues to their worries): pregnant animals, lactating dogs and queens, growing pups and kittens and performance animals (e.g. working dogs, show dogs and cats, sporting dogs and obedience dogs).
Sanitation. Making sure that kennels, catteries and runs are cleaned and sanitary goes a long way towards reducing stress. Kennels and runs must be cleaned twice to three-times daily (or more, if possible). Animals
do not like sitting in feces and urine any more than you do. Excrement promotes the
spread of coccidia and also the growth and spread of other diseases and infections that the animal's immune system must then fight (e.g. bacterial infections). These 'extra' infections divert a portion of the animal's immune system away from fighting diseases such as coccidiosis or parvovirus, which the animal might then, as a result, contract (i.e. the animal's
immune system may have been able to defeat the coccidia or parvo organisms, had
it not also been engaged in fighting off the diseases caused by the lack of sanitation). Remember that good sanitation is particularly important in animals that have other stresses (you don't want to add sanitation issues to their worries): pregnant pets, lactating breeders, growing puppies and kittens and performance animals (e.g. working dogs, sporting dogs and obedience dogs).
Exercise and mental stimulation. Animals get stressed when they are bored and
unstimulated and have no opportunity to occupy themselves. Dogs and felines are intelligent creatures
which need stimulation, both mentally and physically. Dogs in large dog facilities
should be walked a minimum of twice daily (ideally for 30 minutes or more at a time)
and be given room to run around in and toys or other nice dogs to play with (provided they
all get on OK). Cats should be provided with ample space to run around in and toys and climbing frames
and other nice cats to play with (provided they all get on OK). Bitches and queens with newborn litters generally don't like to interact with other dogs or cats
or to be taken away from their offspring and so they should be offered toys and a moderate amount
of space and allowed to choose their activities for themselves.
Stress-relief for late-pregnant and lactating bitches and queens. In the wild, these animals usually go off on their own (into a dark den) to give birth and to rear their litters in private (at least for the first 6 weeks). In a breeding facility, these animals should be allowed their privacy: a warm, well-bedded
dimly-lit place to give birth and rear their pups and kits. These animals should not be placed
in close proximity (sight, smell or hearing) to other dogs and cats and should not be forced
to socialize or leave the newborns too often. This causes stress.
Avoid overcrowding. Yes, I know I have mentioned it 3 times now. This shows how important I think it
is in the prevention of coccidiosis and other diseases. Overcrowding promotes rapid infectious disease spread from animal to animal; it
promotes stress which suppresses the immune response of susceptible animals and overcrowding makes it
difficult for facility operators to find a place, sufficiently out of the way, to isolate the sick.
Be aware of dog-to-dog and cat-to-cat and cat-to-dog interactions. Some animals do not like being housed near other animals for many reasons: simple dislike, prior experiences, the other dog or cat making threatening gestures at them through the fence (rigid stance, growling, staring etc). Placing an animal
for long periods of time in close proximity to an animal that it fears or does not get along
with will inevitably lead to stress. Dogs and cats may not realise (as we do) that the big dog
next door can not get at them through the fence. Thus, leaving those animals side
by side (especially in wire-fenced cages where they can clearly eye each other) will
result in one animal being in constant fear that the other will soon attack them.
Ideally, only place animals in close proximity that get along or are at least indifferent to each other.

11. How to disinfect the environment following feline and canine coccidia contamination.
Regardless of whether an affected coccidia case appears in your own home or in a larger multiple-dog or multiple-cat environment such as a breeding facility or veterinary clinic, it is important that correct measures are taken to clean and disinfect the contaminated areas.
Chemical agents (disinfectants) used to kill coccidia organisms.
Coccidial oocysts that contaminate an environment are notoriously resistant to most disinfectant chemicals. In fact, some texts even go so far as saying that there is no
chemical disinfectant that is 100% reliable at completely removing infective coccidial oocysts
from an environment and that all we can hope for is for the disinfectant to reduce the numbers of oocysts down to minimally infectious levels (reduce the environmental
burden). The following sections list the chemicals and protocols that have been found to have some
effect at killing coccidial organisms (including Toxoplasma).
Initial cleaning with water.
Before a disinfectant can be used on an area, it is important to thoroughly scrub the
area with water beforehand. This is to remove any gross pus, fecal, urine, vomit and soil matter from the surfaces. It is important to do this because organic matter such as feces can inhibit the effects of some disinfectants (for example QUATs)
and even deactivate them! Removing fecal and soil/dust matter will also reduce the surface area over which the coccidia oocysts can hide out, thereby enhancing the ability of the disinfectants to make contact with them and kill them.
This initial cleaning process should not contain disinfectants or other soaps because some
disinfectants will react badly with or deactivate other kinds of disinfectants (the reaction can even create poisonous gasses which you might breathe in).
Ammonia.
Most texts that discuss the disinfection of coccidia contamination in dog, cat and livestock facilities recommend that a solution of 10% ammonia (a very high concentration) be applied
to infected surfaces. This solution can be left to dry and stand overnight.
Ammonia solutions release nasty, irritant, noxious vapors that irritate the airways, nasal passages and lungs of people and animals. Ammonia should, ideally, only be used in well-ventilated areas or, if used in poorly ventilated areas, with appropriate safety apparatus (face and eye masks, possibly even breathing apparatus). High ammonia
concentrations can also cause nasty chemical burns if animals are directly exposed to
them. Animals must never be allowed to consume ammonia.
Once applied and given time to act (e.g. left overnight), ammonia solutions must be rinsed thoroughly, leaving no residues, and the area allowed to ventilate well before animals can be reintroduced.
Phenolic compounds.
The phenolic compounds have also been suggested in some texts as a way of decontaminating coccidia-affected premises. Phenols are of particular
benefit in kennelling and cattery situations since they are not deactivated by other soaps or organic
soil and faecal matter. Like most of the disinfectants discussed on this page, phenolic
compounds can leave skin and mucous-membrane irritant residues: surfaces cleaned with
them should be rinsed thoroughly after application (prior to reintroduction of animals). This is particularly important in feline premises and premises with large populations of neonates (newborns): cats
and newborn litters are very susceptible to the toxic effects of phenolics.
For those of you looking for effective, biodegradable, non-toxic chemicals, there is a new compound put out by the Nutribiotic company called Citricidal (ref. Greene CE). This is a natural diphenol derived from grapefruit
seed.
Non-chemical agents used to kill coccidia.
The best way to kill coccidial organisms is with heat: boiling water or steam or sunlight
(though natural sunlight exposure takes weeks to months to kill coccidia). Most of
the texts that discuss coccidial decontamination of a premises suggest using steam cleaning or
boiling water as the main method of decontamination. Not only are these techniques the most effective means of reducing oocyst numbers, they are also devoid of harmful residues and vapours.
Steam-cleaning.
Most infectious disease organisms, including resistant heavy-weights such as parvovirus
and coccidia, are susceptible to the effects of intense heat and pressure. Steam applied under
pressure (steam cleaning) is the most effective means of achieving sterility (Greene). Steam cleaning can be used in cages, dog runs, concreted areas and tiled regions and may be an option for carpets, clothing and bedding where other chemical compounds might not be appropriate. Autoclaving (whereby hospitals and vet clinics use intense pressure and heat to sterilize surgical equipment) is a good way of removing infectious organisms from steel fomites, instruments and cloth materials.
Bowman (reference 13) recommends the following method for decontaminating farrowing
crates (piggery cages), a technique which could easily be applied to dog and cat facilities:
steam clean the farrowing crates; then wet the crates down with a 10% ammonia
or phenolic disinfectant compound; let it stand overnight and then rinse the crates
thoroughly and repeat the steam cleaning again the next day.
Boiling water.
Boiling your drinking water has long been a tried and true method of destroying parasites
present in natural waterways (e.g. Cryptosporidium, Giardia) and fouled drinking water supplies.
Immersing steel fomites (e.g. dog bowls, water dishes), surgical instruments and fecally contaminated clothing in rolling boiling water for 15-30 minutes should kill any coccidial organisms present. It is a simple, easily available, cheap and effective
way of removing infectious coccidial organisms from steel fomites, instruments and cloth materials.
Depopulation and resting the environment.
Sunlight, heat and dry, desiccating conditions will eventually kill coccidial organisms, although this takes time. Simply removing all animals from a premises, disinfecting the premises well and leaving the premises unpopulated for several months may
be a useful way of reducing coccidial contamination. This technique will probably not work in cold or freezing
climates because oocysts are very resistant to freezing.
Remove the infected surfaces.
This is an expensive way to remove infectious disease organisms, however it does work. Routinely replacing gravel, topsoil or lawn surfaces that have become contaminated and replacing them with new, fresh, non-contaminated surfaces is an excellent way to
remove infectious disease organisms, particularly long-lived organisms such as parvovirus
and coccidia. If the difficult-to-clean surfaces (soil, lawn etc) can be replaced with new, easy-clean surfaces such as concrete or tiles or
metal (in the case of runs and cages), so much the better.

12. Removing coccidia cysts from contaminated meat:
Infectious coccidia cysts (including the cysts of zoonotic, highly-infectious, coccidia-related organisms such as
Toxoplasma) can be contracted by dogs and cats (and man) through the consumption of undercooked meat
and offal (particularly the liver and brains). A wide range of wild and livestock animal
species commonly fed to pets by their owners can carry these cysts, including cattle, sheep, goats, pigs, deer, kangaroos and horses.
Owners can prevent their pets from ingesting meat-borne coccidial cysts by not feeding their
pets raw meat or offal. Thorough cooking destroys the cysts, along with a range of other nasty, meat-associated, bacterial and parasitic pathogens, and is the safest way of feeding
meat or offal to animals.
Owners that prefer (or insist upon) feeding raw meat products
to their animals should only purchase human-quality meat products for their pets. These meat and offal products have been thoroughly checked out by abattoir officers and deemed safe for human (and pet) consumption. Such abattoir-approved products should, hopefully,
not contain any nasties such as hydatid cysts. Owners should never feed
self-killed, raw meat or offal to their pets (e.g. kangaroos and sheep killed through
hunting activities) because most owners are not skilled at recognizing diseased
organs and muscles and might inadvertently feed these to their pets.
Any meat, bones and offal purchased for animal consumption (that owners plan not to cook) should be
frozen in the freezer for a minimum of 3 weeks before defrosting them and feeding them to their pets. Freezing will kill any encysted coccidial parasite cysts.

13. Coccidia and coccidiosis - a summary of the important points:
1) Coccidiosis is a common, highly contagious disease characterized by watery to custard-consistency (mucoid) diarrhoea
and the production of mucoid, jelly-like faeces with or without the presence of blood (hematochezia). Animals with non-complicated cases of coccidiosis are usually bright and alert and well-looking and still eating. Vomiting is not a typical presenting sign, but can be present.
2) Coccidiosis is caused by a number of infectious protozoan organisms, Isospora being the most common.
3) Coccidia transmission typically occurs when individual dogs and cats are introduced into environments
with large numbers of other dogs and cats (e.g. kennels, pounds, shelters etc.). The disease is normally spread by the consumption of faeces and fecally contaminated foods, water bowls
and surfaces. Certain species of coccidia are transmitted to dogs and cats through the consumption of non-cooked herbivore or vermin meat and innards (offal or organs).
4) Coccidia are generally host-specific, seldom affecting species of animals
that are unrelated to their usual definitive and intermediate host animal species.
5) Coccidiosis is exacerbated by a range of non-infectious disease factors, including
stress and immunosuppressive diseases and drugs.
6) Coccidiosis (the clinical disease) can become complicated by secondary bacteria, leading to severe
cases of bacterial enteritis and sepsis especially in young or severely immune-suppressed animals.
7) Coccidiosis is normally diagnosed on fecal floatation.
8) Treatment for coccidiosis involves giving the affected animal anticoccidial drugs and other supportive remedies and medications (antibacterial antibiotics, intravenous fluids etc.)
and isolating the animal during the clinical stages of infection.
9) Coccidial drugs may not cure the animal of the parasite. Often the coccidiostatic drugs only act to suppress the symptoms of coccidiosis (shorten the period of clinical disease) until the animal's own immune system responds and suppresses the infection. It is common for a carrier state to develop, whereby the host's immune system suppresses the organism's replication (stops
it from producing clinical signs), but does not clear it from the body.
10) Non-clinical carriers of coccidia are common in the dog and cat population. They shed infective
oocysts into their faeces, which are infective to other, susceptible animals.
11) Adult animals with recurrent or persistent (chronic) symptoms of coccidiosis
should be examined for an underlying immune suppressive disease or an alternative intestinal
disease that is either mimicking coccidiosis or exacerbating a pre-existing coccidial disease
condition.
12) It is rare for coccidia infected animals to die from the disease. Young puppies, very old animals, animals with pre-existing debilitation and immune suppressed animals
are most at risk of secondary complications that could result in severe disease and even death.
13) No vaccine is available for coccidia.
14) Good sanitation and hygiene practices are essential to preventing and controlling
outbreaks and endemics of these organisms.
15) Coccidiosis is quite resistant to a wide range of disinfectants and environmental conditions. Steam cleaning is the best way of removing
coccidia from a premises.
16) Sarcocystis neurona is a newly recognised (emerging) coccidial disease that affects the brains of
horses and cats.

To go from our coccidiosis in dogs and cats page to our homepage, click here.

References and Suggested Readings:
1) General Therapeutic Principles. In Nelson RW, Couto CG, editors: Small Animal Internal Medicine, Sydney, 1998, Mosby Inc.
2) Dubey JP, Greene CE,Enteric Coccidiosis. In Greene CE, editor: Infectious Diseases of the Dog and Cat, St. Louis, 2006, Saunders Elsevier.
3) Greene CE, Ewing SA, Antiprotozoal Chemotherapy. In Greene CE, editor: Infectious Diseases of the Dog and Cat, St. Louis, 2006, Saunders Elsevier.
4) Greene CE, Environmental Factors in Infectious Disease. In Greene CE, editor: Infectious Diseases of the Dog and Cat, St. Louis, 2006, Saunders Elsevier.
5) Lawler DF, Prevention and Management of Infection in Kennels. In Greene CE, editor: Infectious Diseases of the Dog and Cat, St. Louis, 2006, Saunders Elsevier.
6) Greene CE, Gastrointestinal and Intraabdominal Infections. In Greene CE, editor: Infectious Diseases of the Dog and Cat, St. Louis, 2006, Saunders Elsevier.
7) Little SE, Laboratory Diagnosis of Protozoal Infections. In Greene CE, editor: Infectious Diseases of the Dog and Cat, St. Louis, 2006, Saunders Elsevier.
8) Greene CE, Watson ADJ, Antibacterial Chemotherapy. In Greene CE, editor: Infectious Diseases of the Dog and Cat, St. Louis, 2006, Saunders Elsevier.
9) Antimicrobial Drugs. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
10) Sterilisation and Disinfection. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
11) Host-Parasite Relationships. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
12) Sources and Transmission of Infectious Agents. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
13) Protozoans. In Bowman DD, Lynn RC, Eberhard ML editors: Parasitology for Veterinarians, USA, 2003, Elsevier Science.
14) Diagnostic Parasitology. In Bowman DD, Lynn RC, Eberhard ML editors: Parasitology for Veterinarians, USA, 2003, Elsevier Science.
15) Hulst F, Amphibian Care and Medical Management. In Wildlife in Australia: Healthcare and Management - PGF Proceedings 327, Sydney, 1999, Post Graduate Foundation in Veterinary Science.
16) Booth R, Monotremes. In Wildlife in Australia: Healthcare and Management - PGF Proceedings 327, Sydney, 1999, Post Graduate Foundation in Veterinary Science.
17) Lynch M, Pinnipeds. In Wildlife in Australia: Healthcare and Management - PGF Proceedings 327, Sydney, 1999, Post Graduate Foundation in Veterinary Science.
18) Rose K, Common Diseases of Urban Wildlife. In Wildlife in Australia: Healthcare and Management - PGF Proceedings 327, Sydney, 1999, Post Graduate Foundation in Veterinary Science.
19) Bellamy, T First Aid for Native Flora. In Wildlife in Australia: Healthcare and Management - PGF Proceedings 327, Sydney, 1999, Post Graduate Foundation in Veterinary Science.
20) Blyde D, Advances in Treating Diseases of Macropods. In Wildlife in Australia: Healthcare and Management - PGF Proceedings 327, Sydney, 1999, Post Graduate Foundation in Veterinary Science.
21) Disorders of the Intestinal Tract. In Nelson RW, Couto CG, editors: Small Animal Internal Medicine, Sydney, 1998, Mosby Inc.
22) Hall EJ, Simpson KW, Diseases of the Small Intestine. In Ettinger SJ, Feldman EC, editors: Textbook of Veterinary
Internal Medicine, Sydney, 2000, WB Saunders Company.
23) Lappin MR, Protozoal and Miscellaneous Infections. In Ettinger SJ, Feldman EC, editors: Textbook of Veterinary
Internal Medicine, Sydney, 2000, WB Saunders Company.
24) Levy J, The Fading Kitten and Neonate. In Rand J, editor: Problem-based Feline Medicine, Sydney, 2006, Elsevier Saunders.
25) Zoran DL, The Cat with Signs of Acute Small Bowel Diarrhea. In Rand J, editor: Problem-based Feline Medicine, Sydney, 2006, Elsevier Saunders.
26) Zoran DL, The Cat with Signs of Chronic Small Bowel Diarrhea. In Rand J, editor: Problem-based Feline Medicine, Sydney, 2006, Elsevier Saunders.
27) Diseases and Clinical Syndromes. In Tilley LP, Smith FWK: The 5 Minute Veterinary Consult, Baltimore, 1997, Williams and Wilkins.
28) http://www.capcvet.org/downloads/Coccidiaimages.pdf
29) Antimicrobial Drug Formulary - Appendix 8. In Greene CE, editor: Infectious Diseases of the Dog and Cat, St. Louis, 2006, Saunders Elsevier.
30) Amprolium. In Plumb DC: Plumb's Veterinary Drug Handbook, 5th ed. USA, 2005, Blackwell Publishing.
31) Furazolidone. In Plumb DC: Plumb's Veterinary Drug Handbook, 5th ed. USA, 2005, Blackwell Publishing.
32) Quinacrine. In Plumb DC: Plumb's Veterinary Drug Handbook, 5th ed. USA, 2005, Blackwell Publishing.

Pet Informed is not in any way affiliated with any of the companies whose products
appear in images or information contained within this article. The images, taken by Pet Informed, are only used in order to illustrate certain points being made in the article.
Copyright May 17, 2008, www.pet-informed-veterinary-advice-online.com.
All rights reserved, protected under Australian copyright. No images or graphics on this Pet Informed website may be used without written permission of their owner, Dr. O'Meara.
Clavulox, Clavulox Drops, VibraVet and VibraVet Paste are registered trademarks of Pfizer Animal Health.
Baytril and Baycox are registered trademarks of Bayer Australia Ltd.
Orbax is a registered trademark of Schering-Plough Animal Health.
Trivetrin and Tribrissen are registered trademarks of Jurox Pty Ltd.
Augmentin is a registered trademark of GlaxoSmithKline.
Noroclav is a registered trademark of Norbrook.
Coccivet is a registered trademark of Vetafarm.
Metrogyl is a registered trademark of Alphapharm.
Metronidazole BP is a product of Baxter.
Metrin is a registered trademark of Parnell Laboratories (Aust) Pty Ltd.
Flagyl is a registered trademark of Aventis.
Fecalyzer is a registered trademark of Vetoquinol.
Please note: the aforementioned coccidial treatment schedules and coccidial
prevention guidelines and information on the coccidial diseases of dogs and cats are general recommendations only. The information provided is based on published information and recommendations made available from the drug companies themselves; relevant veterinary literature
and publications and my own experience as a practicing veterinarian.
The advice given is appropriate to the vast majority of pet owners, however, given
the large range of drug types and prevention protocols now available, owners should take it upon themselves to ask their own veterinarian what treatment and disease prevention schedules s/he is using so as
to be certain what to do. Owners with specific circumstances (high coccidia
contamination in their environment, pregnant bitches and queens, breeders, multiple-dog and cat environments,
animals on immune-suppressant medicines, animals with immunosuppressant diseases or conditions
etc. etc.) should ask their vet what the safest and most effective protocol is for their situation.
Any dose rates mentioned on these pages should be confirmed by a vet. Dosing rates for common
drugs are being changed and updated all the time (e.g. as new research comes in and as drug
formulations change) and information here may not remain current for long. What's more, although we try very hard to maintain the accuracy of our information, typos and oversights do occur. Please check with your vet before dosing any pet any medication or drug.
Common coccidia misspellings:
cocsidia, cocsidiosis, cocksidia, cocksidiosis, cokcidia, cokcidiosis, coksidia, coksidiosis, coccidyosis, coccidya, cocsidya, cocsidyosis, cocksidya, cocksidyosis.


 Coccidia is a general term for a range of microscopic protozoan parasites that inhabit
the intestines and, occasionally, other bodily organs of animals and humans. The
information contained within this page provides information and advice on the common intestinal coccidian species (Isospora, Hammondia, Besnoitia and Sarcocystis) known to cause gastrointestinal disease, enteritis and symptoms of weight loss, dehydration, diarrhea, mucoid and bloody feces, straining to defecate and, occasionally, vomiting in puppies and kittens. If your vet has performed a fecal float on the faeces of your kitten or puppy and diagnosed your pet with coccidia or coccidiosis - this is the page for you.
Coccidia is a general term for a range of microscopic protozoan parasites that inhabit
the intestines and, occasionally, other bodily organs of animals and humans. The
information contained within this page provides information and advice on the common intestinal coccidian species (Isospora, Hammondia, Besnoitia and Sarcocystis) known to cause gastrointestinal disease, enteritis and symptoms of weight loss, dehydration, diarrhea, mucoid and bloody feces, straining to defecate and, occasionally, vomiting in puppies and kittens. If your vet has performed a fecal float on the faeces of your kitten or puppy and diagnosed your pet with coccidia or coccidiosis - this is the page for you.  Dogs and cats of any age are able to ingest infectious coccidian parasites and have them
replicate within their intestinal tracts. Whether or not this coccidian infection actually results in any symptoms of disease (diarrhoea etc.), however, has a lot to do with
the age and immune system integrity of the animal host. Coccidian oocysts (the infectious
parasitic cysts shed in the host-animal's faeces) can often be found in the feces of older cats and dogs without these animals showing any signs of disease. Typically, coccidiosis disease symptoms are only seen
in very young puppies and kittens (under 4 months old) whose immune systems are not
yet mature enough to manage and control the parasitic invaders.
Dogs and cats of any age are able to ingest infectious coccidian parasites and have them
replicate within their intestinal tracts. Whether or not this coccidian infection actually results in any symptoms of disease (diarrhoea etc.), however, has a lot to do with
the age and immune system integrity of the animal host. Coccidian oocysts (the infectious
parasitic cysts shed in the host-animal's faeces) can often be found in the feces of older cats and dogs without these animals showing any signs of disease. Typically, coccidiosis disease symptoms are only seen
in very young puppies and kittens (under 4 months old) whose immune systems are not
yet mature enough to manage and control the parasitic invaders.  Disease symptoms, when they occur, tend to occur most frequently in young animals, particularly those that are under conditions of high stress, are malnourished
or are infected with other diseases (e.g. other intestinal parasites) or subjected to poor environmental
conditions. For example, coccidiosis is very common in baby, hand-raised marsupials (e.g.
baby wallabies, possums and kangaroos) because they are suffering from the severe stresses of altered diet (sometimes even an inappropriate diet), human handling and loss of their mother.
Severe clinical infestations are also commonly encountered when the juvenile animal first starts to graze pasture (e.g. around 10 months of age in wombats): it is thought that these animals are being exposed to large amounts of coccidia in the pasture, but have not yet developed good enough anti-coccidial intestinal immunity to deal with it. Consequently, the organisms are permitted to replicate freely and these animals develop symptoms of disease. Some wild animal species (e.g. frogs) seem to suffer very little from their enteric coccidial infections, rarely showing any symptoms of disease, whereas other species
(seals, marsupials, echidnas) may often develop severe disease, even death. For example, echidnas often die from a form of coccidiosis that disseminates from their intestines throughout their
internal organs.
Disease symptoms, when they occur, tend to occur most frequently in young animals, particularly those that are under conditions of high stress, are malnourished
or are infected with other diseases (e.g. other intestinal parasites) or subjected to poor environmental
conditions. For example, coccidiosis is very common in baby, hand-raised marsupials (e.g.
baby wallabies, possums and kangaroos) because they are suffering from the severe stresses of altered diet (sometimes even an inappropriate diet), human handling and loss of their mother.
Severe clinical infestations are also commonly encountered when the juvenile animal first starts to graze pasture (e.g. around 10 months of age in wombats): it is thought that these animals are being exposed to large amounts of coccidia in the pasture, but have not yet developed good enough anti-coccidial intestinal immunity to deal with it. Consequently, the organisms are permitted to replicate freely and these animals develop symptoms of disease. Some wild animal species (e.g. frogs) seem to suffer very little from their enteric coccidial infections, rarely showing any symptoms of disease, whereas other species
(seals, marsupials, echidnas) may often develop severe disease, even death. For example, echidnas often die from a form of coccidiosis that disseminates from their intestines throughout their
internal organs.  A number of species of Isospora are known to infect our domestic pets, in particular:
Isospora felis and Isospora rivolta in the cat and Isospora canis, I. neorivolta, I. ohioensis and I. burrowsi in the dog. This parasite species (Isospora) has no intermediate host requirement and is able to spread from cat to cat and dog to
dog via direct fecal-oral transmission. It is highly contagious. Kittens and puppies (and older animals)
become infected if they consume Isospora-contaminated feces from other cats or dogs and may even reinfect themselves through the consumption of their own Isospora-infected droppings. This is one reason
why owners should not let their dogs and cats consume the stools of other animals.
It is also a reason why dog and cat food and water bowls should not be placed in a position
whereby the food and water could become contaminated with fecal material (e.g. pets stepping into food and water dishes with their poop-covered feet) and, subsequently, consumed.
A number of species of Isospora are known to infect our domestic pets, in particular:
Isospora felis and Isospora rivolta in the cat and Isospora canis, I. neorivolta, I. ohioensis and I. burrowsi in the dog. This parasite species (Isospora) has no intermediate host requirement and is able to spread from cat to cat and dog to
dog via direct fecal-oral transmission. It is highly contagious. Kittens and puppies (and older animals)
become infected if they consume Isospora-contaminated feces from other cats or dogs and may even reinfect themselves through the consumption of their own Isospora-infected droppings. This is one reason
why owners should not let their dogs and cats consume the stools of other animals.
It is also a reason why dog and cat food and water bowls should not be placed in a position
whereby the food and water could become contaminated with fecal material (e.g. pets stepping into food and water dishes with their poop-covered feet) and, subsequently, consumed.
 The main species of enteric Coccidia infecting kittens and puppies is Isospora:
Another thing to be aware of, when it comes to Isospora-infected faeces, is that faeces
infected with this organism do not have to look abnormal and nor do they have
to come from a kitten or puppy. Isospora is not only found
in obviously-diseased, slimy, bloody-looking diarrhoea specimens (e.g. the image on the right). The organism can be found in perfectly formed, normal-looking faeces produced by subclinically infected kittens,
puppies and adult animals. Coccidia carriers (animals that have the infection and are shedding
the organisms in their faeces, but which show absolutely no symptoms of disease) are very common
in the dog and cat population and their faeces, though normal-looking, can be highly infective to other, more-susceptible animals.
The main species of enteric Coccidia infecting kittens and puppies is Isospora:
Another thing to be aware of, when it comes to Isospora-infected faeces, is that faeces
infected with this organism do not have to look abnormal and nor do they have
to come from a kitten or puppy. Isospora is not only found
in obviously-diseased, slimy, bloody-looking diarrhoea specimens (e.g. the image on the right). The organism can be found in perfectly formed, normal-looking faeces produced by subclinically infected kittens,
puppies and adult animals. Coccidia carriers (animals that have the infection and are shedding
the organisms in their faeces, but which show absolutely no symptoms of disease) are very common
in the dog and cat population and their faeces, though normal-looking, can be highly infective to other, more-susceptible animals. 

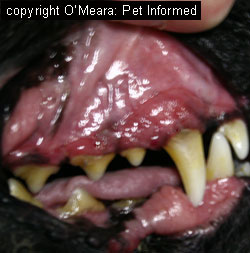



 As mentioned previously, most coccidia species are host specific when it comes to the types of
animals whose intestines and colons they will infect. An oocyst belonging to a cat- or pig-adapted
coccidian organism will not hatch in a dog intestine and nor will it replicate to cause symptoms of intestinal disease in a dog. Instead, should a dog consume the droppings
of a coccidia-infected non-canine species of animal (e.g. a dog that regularly consumes pig poo or cat droppings),
any oocysts ingested will pass through the dog's intestines unhatched and come out, unharmed,
in the stools of that dog. A veterinarian who subsequently performs a fecal flotation on that dog's droppings may misdiagnose that dog as having coccidiosis should
he or she fail to recognize that the coccidial oocysts seen are not of the dog-infectious variety.
Similar to the situation described in point 1 of this section, symptoms of intestinal disease
seen in this kind of patient will not respond to coccidiosis treatment because the coccidian
organisms found in the stools are not the cause of the issue. The animal will continue to show abnormal intestinal symptoms (the coccidiosis will seem to 'persist') until the true
intestinal issue is diagnosed.
As mentioned previously, most coccidia species are host specific when it comes to the types of
animals whose intestines and colons they will infect. An oocyst belonging to a cat- or pig-adapted
coccidian organism will not hatch in a dog intestine and nor will it replicate to cause symptoms of intestinal disease in a dog. Instead, should a dog consume the droppings
of a coccidia-infected non-canine species of animal (e.g. a dog that regularly consumes pig poo or cat droppings),
any oocysts ingested will pass through the dog's intestines unhatched and come out, unharmed,
in the stools of that dog. A veterinarian who subsequently performs a fecal flotation on that dog's droppings may misdiagnose that dog as having coccidiosis should
he or she fail to recognize that the coccidial oocysts seen are not of the dog-infectious variety.
Similar to the situation described in point 1 of this section, symptoms of intestinal disease
seen in this kind of patient will not respond to coccidiosis treatment because the coccidian
organisms found in the stools are not the cause of the issue. The animal will continue to show abnormal intestinal symptoms (the coccidiosis will seem to 'persist') until the true
intestinal issue is diagnosed.  Faecal flotation is a test performed on the faeces of the clinically infected or carrier dog and cat, or any other animal species that is a definitive host for some species of intestinal coccidian. The test is performed in order to detect the presence of tell-tale coccidial oocysts in the faeces
of the infected animal, thereby supporting a diagnosis of coccidiosis. The test can also
be used to detect the fecally-shed oocysts of certain other parasitic protozoan organisms, including Toxoplasma, Cryptosporidium and Giardia, as well as the eggs of various parasitic worms, including whipworm, tapeworm, roundworm and hookworm.
Faecal flotation is a test performed on the faeces of the clinically infected or carrier dog and cat, or any other animal species that is a definitive host for some species of intestinal coccidian. The test is performed in order to detect the presence of tell-tale coccidial oocysts in the faeces
of the infected animal, thereby supporting a diagnosis of coccidiosis. The test can also
be used to detect the fecally-shed oocysts of certain other parasitic protozoan organisms, including Toxoplasma, Cryptosporidium and Giardia, as well as the eggs of various parasitic worms, including whipworm, tapeworm, roundworm and hookworm. 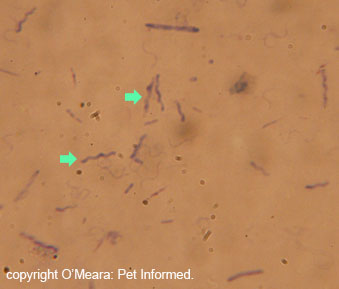
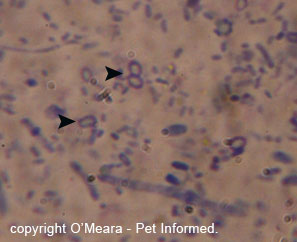

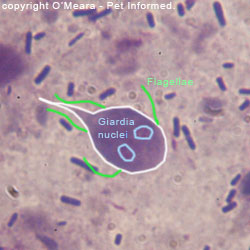
 Trimethoprim and sulfonamide are two individual antibiotic drugs that have been found to have
synergistic properties (enhanced organism killing properties) when they are used together. These drugs are the first choice (drugs of choice) for coccidiosis treatment
and are thought to be less toxic than many of the other antimicrobial chemicals used for this purpose.
Trimethoprim and sulfonamide are two individual antibiotic drugs that have been found to have
synergistic properties (enhanced organism killing properties) when they are used together. These drugs are the first choice (drugs of choice) for coccidiosis treatment
and are thought to be less toxic than many of the other antimicrobial chemicals used for this purpose.
 Amprolium is another anticoccidial remedy that can be used to treat coccidiosis in dogs and cats. As seen in the product image (right), it is also one of the more common medications used
to treat coccidiosis in birds.
Amprolium is another anticoccidial remedy that can be used to treat coccidiosis in dogs and cats. As seen in the product image (right), it is also one of the more common medications used
to treat coccidiosis in birds.  Toltrazuril is another anticoccidial drug that is commonly be used to treat coccidiosis in dogs and cats. As seen in the product image (right), it is also one of the more common medicines used
to treat coccidiosis in piglets.
Toltrazuril is another anticoccidial drug that is commonly be used to treat coccidiosis in dogs and cats. As seen in the product image (right), it is also one of the more common medicines used
to treat coccidiosis in piglets.






 Plasma is the fluid that remains when you remove all of the cells from blood. It contains
several helpful substances that can really make a huge difference to the survival chances of coccidia puppies and kittens.
Plasma is the fluid that remains when you remove all of the cells from blood. It contains
several helpful substances that can really make a huge difference to the survival chances of coccidia puppies and kittens.  Some patients lose so much blood as a result of gastrointestinal and colonic ulceration that they
can actually become severely anemic in addition to losing protein into the gut.
Some patients lose so much blood as a result of gastrointestinal and colonic ulceration that they
can actually become severely anemic in addition to losing protein into the gut.