Veterinary Advice Online: Canine Distemper.
 The information contained within this article covers a range of canine distemper topics written to fully educate pet owners about distemper virus in dogs (ferrets are also discussed). The canine distemper information presented here is detailed (but still easy to understand) because we are aiming to educate owners thoroughly and provide them with enough information that they might be better informed and able to troubleshoot problems with their own pets. The topics are covered in the following order:
The information contained within this article covers a range of canine distemper topics written to fully educate pet owners about distemper virus in dogs (ferrets are also discussed). The canine distemper information presented here is detailed (but still easy to understand) because we are aiming to educate owners thoroughly and provide them with enough information that they might be better informed and able to troubleshoot problems with their own pets. The topics are covered in the following order:
1) What is distemper? - this short section comprises a basic definition about what dog distemper is.
2) Which animals are at risk of distemper?
3) How do animals catch canine distemper? - this section contains information about where and how animals can catch canine distemper; the high risk environments and whether distemper vaccines can cause disease.
4) What does distemper do to your dog? This section contains the following subsections:
4a) How do canine distemper viruses work (how do they replicate and destroy cells etc.)
4b) How does canine distemper affect the bone marrow, lymphatic tissues and blood cells?
4c) How does canine distemper affect the intestine?
4d) How does canine distemper affect the respiratory tract and mucous membranes?
4e) How does canine distemper affect the brain?
4f) How does canine distemper affect the skin?
4g) How does canine distemper affect the eye and other organs?
4h) How canine does distemper affect the joints and bones?
4i) Can animals show minimal or no disease signs of distemper?
4j) Distemper vaccine-associated disease.
5) How is distemper diagnosed? This section discusses the methods of testing for distemper and their pros and cons.
5a) General blood panels.
5b) Blood smears - visualising viral inclusion bodies.
5c) Canine distemper antibody measurements.
5d) Canine distemper antibodies in brain and eye fluid.
5e) CSF tap.
5f) Tissue samples.
5g) Tests of the future - PCR and tissue culture.
6) How is distemper treated?
7) What is the prognosis for distemper?
8) How to prevent distemper? - this section contains general advice on prevention of canine distemper virus for pet owners and includes information on vaccination schedules and vaccine protocols.
9) How to prevent distemper in high risk situations? - this section contains useful tips and hints for preventing canine distemper virus infection and spread in situations with high viral contamination (e.g. contaminated breeding facilities, contaminated homes).
10) How do you disinfect the environment following distemper contamination?
11) Summary and take home messages - a summary of the important points.
WARNING - IN THE INTERESTS OF PROVIDING YOU WITH COMPLETE AND DETAILED INFORMATION, THIS SITE DOES CONTAIN MEDICAL AND SURGICAL IMAGES THAT MAY DISTURB SOME READERS.

1. What is Distemper?
Distemper is a severe, often fatal disease of the brain, gastrointestinal tract, lungs and other organs of dogs and other canids that is caused by a virus called canine distemper virus (we sometimes shorten it to CDV). This virus is a member of the Paramyxoviridae virus family, a family which includes several genera, one of which, the genera
Morbillivirus, contains canine distemper virus. The disease is also known to affect members of the weasel family (including pet ferrets and stoats), foxes, skunks, seals, porpoises and raccoons.
 Typically, canine distemper virus affects the lymphatic system, nervous system, lungs, gastrointestinal tract,urinary tract, eyes and skin of the animal and, as a result, animals generally present with a range of neurological signs, respiratory signs, gastrointestinal signs (vomiting, diarrhea), ocular signs and skin signs. Canine distemper affected animals will also present with non-specific signs of illness: fever, lethargy, inappetence and dehydration. Occasionally, distemper can even affect other, less typical, areas of the body such as the eyes and bones and the appearance of some odd clinical syndromes such as 'dry eye', uveitis (inflammation inside the eye) and HOD (hypertrophic osteodystrophy) can result. All of these symptoms are discussed in section 4 of this article. Importantly, it must be mentioned that not every case of canine distemper presenting to a veterinarian will display all of these organ symptoms at once. Some cases show all of the signs; some only present with respiratory symptoms and some cases might show just neurological signs and nothing else. Some animals show no signs at all (they are subclinically affected). The difference in signs may reflect differences in immunity of the animals and/or differences in the strains of canine distemper in the environment (some strains are very aggressive and prefer to invade the brain, for example).
Typically, canine distemper virus affects the lymphatic system, nervous system, lungs, gastrointestinal tract,urinary tract, eyes and skin of the animal and, as a result, animals generally present with a range of neurological signs, respiratory signs, gastrointestinal signs (vomiting, diarrhea), ocular signs and skin signs. Canine distemper affected animals will also present with non-specific signs of illness: fever, lethargy, inappetence and dehydration. Occasionally, distemper can even affect other, less typical, areas of the body such as the eyes and bones and the appearance of some odd clinical syndromes such as 'dry eye', uveitis (inflammation inside the eye) and HOD (hypertrophic osteodystrophy) can result. All of these symptoms are discussed in section 4 of this article. Importantly, it must be mentioned that not every case of canine distemper presenting to a veterinarian will display all of these organ symptoms at once. Some cases show all of the signs; some only present with respiratory symptoms and some cases might show just neurological signs and nothing else. Some animals show no signs at all (they are subclinically affected). The difference in signs may reflect differences in immunity of the animals and/or differences in the strains of canine distemper in the environment (some strains are very aggressive and prefer to invade the brain, for example).
Given that the canine distemper virus does not persist long in the environment (certainly nowhere near as long as parvo!) and that the current vaccination programmes for the disease have been very successful, it is now exceptionally rare to see cases of clinical distemper disease at all. Most Australian inner city veterinarians with under 10 years of experience will almost certainly have never encountered a case.
Occasionally, outbreaks of canine distemper are encountered in Australia and elsewhere and these usually occur in remote areas (e.g. aboriginal communities and remote country towns) where vaccination programmes have not been maintained or where standards of hygiene and dog control (e.g. many dogs from different households all mixing freely) are not optimum. Very occasionally, we will see outbreaks of canine distemper disease in inner city, very low socioeconomic areas and also in dog breeding facilities and greyhound facilities and, again, this is usually because standards of vaccination, hygiene and quarantine protocols have not been upkept.

2. Which animals are at risk of canine distemper?
Generally young, unvaccinated or not fully-vaccinated puppies, under 6 months of age, are most susceptible to canine distemper virus. Very young puppies (under 3 months old) that did not receive their mother's colostrum (maternal immunity) are also at high risk. Older, unvaccinated dogs can also contract the disease if they are unlucky enough to encounter a sick dog (or ferret), which is shedding distemper, or encounter the rare virus in their local environment. Puppies and older dogs that are vaccinated, but which do not respond adequately towards their vaccinations (fail to mount a protective immune response) are also at risk, as are immune-suppressed pets (pets on chemotherapy etc.) whose immune systems are not capable of responding to the virus organisms. For more information on vaccination failure, see our vaccination failure page for more details.
Puppies and dogs that have not been fully immunized against distemper are at risk of contracting the disease if their owners take them out into public places that have recently been contaminated with distemper virus particles (the virus does not persist long in the environment - so contamination usually has to have been recent) or let them meet and greet other dogs who could potentially be carriers of the virus. Even if not-fully-vaccinated puppies are not taken out of the house, owners can potentially bring the virus home to them (thereby infecting them) by not being sufficiently hygienic (washing hands etc.) following visitations to environments where there has been distemper. Our next section discusses the environmental distemper risks and where dogs get distemper from, in full.
Ferrets and other members of the weasel family are also at risk of contracting distemper, either from the environment or from other sick dogs and ferrets. Similar to the situation seen in dogs, vaccination of these animals is key to prevention of disease. Generally, only unvaccinated ferrets or ferrets that do not respond to vaccination by mounting an adequate immune response (see our vaccination failure page - it applies to ferrets also) will contract this disease.
A number of wild animal species also get the distemper condition (or a closely-related variant), including other members of the weasel family (including pet ferrets and stoats), wolves, coyotes, foxes, skunks, seals, porpoises and raccoons.
Feline distemper?
Contrary to common belief, canine distemper does not affect cats. CDV has been administered to domestic cats experimentally, but no disease signs were seen. The one, notable exception has been in the large felines (lions, panther, leopards, tigers etc.) where canine-form CDV has been known to cause neurological disease.
A lot has been written about 'feline distemper' on the internet, however, the disease that cat fanciers commonly nickname feline distemper or cat distemper is actually a parvo virus disease termed feline panleukopenia. This disease is more closely related to the disease: canine parvovirus (parvo) than it is to canine distemper. For those of you wanting information on feline distemper symptoms and treatment, I refer you to our current page on canine parvovirus for more information while our
cat vaccination information pages are being built. We will be bringing you the cat vaccine pages as soon as we can. Please be patient :-)

3. Where do dogs get canine distemper from?
Canine distemper virus (CDV) is shed into the environment in the vomit, diarrhea, urine, eye secretions and respiratory secretions (saliva, nasal discharges, sputum/phlegm and expectorant - the mucus and aerosolized droplets that explode from the trachea of an animal into the air when it coughs) of an animal that is infected with the disease.

Animals that are unvaccinated or inappropriately vaccine protected can become sick if they ingest vomit, urine, feces, eye or respiratory secretions contaminated with infective distemper virus particles. Even though overt consumption of feces and vomit etc. is highly likely with dogs (they eat pooh all the time!), the ingestion of viral particles by your dog may not be as obvious as this: your pet could inadvertently ingest virus organisms simply from eating out of (apparently clean) feeding dishes and water bowls that have been contaminated by a sick dog's respiratory secretions or vomit. As an owner, you might not even realise that there was contamination present. It is for this reason (the risk of catching infectious diseases) that dogs should not be permitted by owners to consume the droppings, vomitus, urine or body secretions of other animals. The risk of infectious disease transmission is also a reason why owners should be very careful about letting dogs eat and drink from the same unwashed feeding dishes, water troughs and standing water sources (pools, puddles etc.) as other animals.
Dogs and ferrets can also become sick if they inhale the aerosolised respiratory secretions of a distemper dog (or ferret) that has recently coughed or sneezed: every sneeze and cough releases thousands of microscopic droplets of fluid from the respiratory tract into the environment and each droplet can contain thousands of infectious viral particles. The droplets are so small that, when the next dog inhales them, these droplets will penetrate deeply into the smallest air passages of the lungs. The viruses that invade these deep lung regions can set up a nasty lung infection (viral pneumonia).
It is possible for dogs to also ingest infectious distemper viral particles when they lick the shoes, hands or clothes of a human that has been in hands-on contact with an affected animal. Those hands and clothes may look clean, but still contain infectious distemper particles. Biting and licking the fur of infected animals may also result in infection. Infected animals spread virus particles onto their fur through rolling or lying in feces or through licking their bodies (virus from the respiratory and vomit secretions is transferred onto the coat in this way). Even taking an under vaccinated dog for a walk (e.g. on public surfaces, lawns, parks etc.) could result in infection: your dog could walk across contaminated ground containing vomitus or feces and come home, lick its feet, and get infected.
What must be noted however, particularly with concern to the last paragraph, is that distemper (unlike parvo) is actually quite a short-lived virus in the environment (around 20 minutes up to 180 minutes in warm climates). It is a fragile enveloped virus (this will be discussed in the next section) and this enveloped structure means that the distemper organism is very susceptible to heat, sunlight, desiccation (drying out) and most soaps and disinfectants. Consequently, a human owner that takes basic hygiene precautions (thoroughly washes his hands and clothes with soap) should not pass infectious particles onto his puppy or ferret. Likewise, although distemper particles can be shed into the general environment in the feces and vomit etc. of infected animals, the virus should not last very long in most open environments (parks etc.). Consequently, it would be quite rare for a unvaccinated dog to catch distemper simply by walking in the park or on a footpath, unless the contamination of the environment with excrements was very fresh and recent (you'd have to be unlucky).
The one exception comes with cold climates (not generally experienced in Australia). In conditions close to freezing (4C or less), the virus may survive for weeks in the environment. This is a consideration for those of you who come from cold climates or who have kennels and breeding facilities in cold climates. You will need to be more vigilant with regard to disinfecting contaminated premises and with regard to keeping your puppies isolated from infection until they are completely vaccine protected.
As veterinarians, we still advise, of course, that you do not take your puppy out into the public arena or take him out to meet other dogs until after he is fully vaccinated and protected. The main reason for this is that, even though distemper and kennel cough organisms do not generally last long in the environment, the highly contagious parvovirus organism, which we also vaccinate against, does last a long time and any environment could be contaminated it (see our great parvo page for all you need to know about canine parvovirus).
High risk environments:
Obviously, some environments are more risky than others. Environments that are more likely to have had distemper recently (and which are therefore at higher risk of containing infectious particles) include indigenous peoples' encampments, low socioeconomic suburbs (where people might not vaccinate their animals) and certain breeding facilities (these are generally breeding facilities of lower hygiene and disease prevention standards, however, occasionally even a good breeder might get an outbreak). Breeding facilities may sell their infected puppies to pet retailers (pet shops) or take them to vet clinics for treatment and so pet shops and veterinary clinics should also be considered a potential higher-risk source of infection.
It is important to note, however, that pet shops and vet clinics with good hygiene and disinfection standards should not retain infective particles within their premises for long (thus it should still be rare to catch the organism from these environments). The main time that you will see the spread of distemper from dog to dog in places like veterinary clinics comes when the veterinarian or pet shop owner has not recognized the signs of distemper and not thought to isolate the animal from other people's susceptible pets. This sounds horrible, but distemper is, unfortunately, an easy disease to misdiagnose. Distemper is a tricky condition that can present with a wide range of clinical signs (different cases can look very different); can be easily confused with lots of other non-contagious respiratory and neurological diseases and is very difficult to test for definitively (see our distemper testing section - section 5 - for more). As a general precaution, you should protect your unvaccinated puppy wherever possible by keeping him out of contact with surfaces (e.g. flooring) in veterinary clinics and other facilities (e.g. grooming salons) where dogs go. If you have a large breed unvaccinated puppy to take to the vet (large breeds are tricky to keep off the floor), you can reduce your risk of distemper and parvo exposure by using the 'cat entry' side of the clinic (a lot of newer clinics have a cat side and a dog side).
An additional point to mention is that, in the veterinary world, a local outbreak of distemper is usually a very newsworthy event - this is because it is such an uncommon disease. Generally an outbreak of distemper in an inner city or regional area will be reported on and most vets, breeders, dog clubs and pet shops will soon know of it. This fore-knowledge enables vets in the area to more quickly diagnose the disease and to take the appropriate measures of isolation and decontamination needed. Pet shops and informed owners will quickly stop buying from affected premises too. All of these measures, taken quickly, act to reduce the spread of the disease and the contamination of the environment. As an owner looking to buy a new puppy or as an owner planning on taking your pup to a nearby vet clinic, you will most likely find out about a distemper outbreak in good time and be able to avoid buying a puppy from or taking a puppy to an exposed area.
Can vaccines cause distemper?
It is possible for some of the disease syndromes commonly attributed to wild-type, infectious distemper virus to occur when animals are given certain virulent strains of live distemper virus vaccine. It is a rarity and generally only occurs when live vaccines are given inappropriately (e.g. given to pregnant bitches, underage puppies, immune suppressed animals or to animals harbouring other diseases, such as parvo). Vaccine-associated distemper may also occasionally occur when certain susceptible breeds and lines of dog (e.g. certain lines of Weimaraners) are given certain strains of live distemper vaccine. Vaccine-related distemper, and vaccines to be cautious of, are discussed in section 4j. and section 8 (preventing distemper) of this article.

4. What does distemper virus do to the dog? - an overview of distemper symptoms.
As mentioned in the opening sentences, distemper is a viral disease that causes neurological signs, vomiting, diarrhea, pneumonia and respiratory signs, skin lesions, inappetence, fever, lethargy, depression and severe illness in dogs and ferrets afflicted with it. Occasionally, it even causes eye and bone disease. The following discussion is mostly for those of you who are interested in how the virus works in order to infect these organs and create these distemper symptoms. Understanding how the virus works is useful because it aids your understanding of why symptoms occur; how the disease is spread; what treatments are available and why the mortality is so high.
4a. How a distemper virus infects and damages a cell:
A distemper virus is a tiny organism (much smaller than a bacteria) which is made up of a protein shell or capsule (called a capsid) entwined around and protecting a strand of RNA (not DNA). The whole complex (RNA sequence plus its protective capsid) plus additional free-floating proteins and enzymes (including RNA polymerase - see discussion below) is contained within a membrane coating made up of proteins, carbohydrates and lipids (fats).
What is RNA?
You have probably heard of DNA (Deoxyribonucleic Acid). All human cells have DNA. DNA is a sequence of four different kinds molecules (A,T,C,G) which can be arranged in millions of different combinations of varying lengths to code for all of the genes of your body. The information contained in each gene sequence can be used by the cell as a template or set of instructions by which that cell is able to manufacture certain important proteins and molecules vital to cellular function, replication and survival. Every cell in the body has the same DNA (every cell therefore contains every gene in the body), but not every gene contained in the full DNA sequence is switched on (activated) in every cell. Only certain cells use certain genes to guide them in making the proteins necessary for their structure and function. For example: insulin is a protein coded for by a gene sequence contained in the DNA. The insulin gene is only switched on in pancreatic cells and the cells of the pancreas use the information contained in the sequence to enable them to make insulin for the body.
The RNA (RiboNucleic Acid) sequence contained within the distemper virus plays a similar role in the functioning of the virus organism to the role that DNA plays in our own cells. Similar to DNA, RNA is basically just a strand of protein molecules arranged in various combinations (genes) that code for certain proteins and molecules vital to virus function, replication and survival. The viral RNA contains sequences (genes) that code for enzymes (termed RNA polymerase) needed in the replication of more strands of viral RNA; internal viral proteins (such as the virus capsid) and various other virus components, such as surface proteins (the same ones we called antigens in our How Vaccines Work page) which allow the virus to access animal cells.
Unlike bacteria and other, more advanced organisms, viruses do not contain all of the components needed to replicate by themselves. They require a host cell (e.g. a dog cell) which contains all of the right components required for viral replication. For the sake of this discussion, animal cells can be thought of as being comprised of three main regions of viral importance:
1) The cell membrane - the coating (wall) of the cell which acts as a barrier to stop the nucleus and cytoplasm from leaking out and which plays a role in virus attachment and facilitation of virus infection (viruses must attach to the cell membrane first in order to access a cell).
2) The nucleus - a region within the cell that is contained within its own thin membrane. It contains the DNA that codes for all of the functions of the animal cell (see above DNA discussion).
3) The cytoplasm - the 'innards' of the cell that lie outside of the nucleus, but within the main cell membrane. The cytoplasm contains all of the 'equipment' needed to manufacture proteins and molecules vital to cell function: it is the factory of the cell.


The images show a normal dog white blood cell: the important anatomy is of the cell is indicated (cell membrane, nucleus and cytoplasm).
When the distemper virus enters the body of a dog, it attaches to the cell membrane of a particular body-cell-type that it has been specially 'designed' to invade (i.e. the virus has surface proteins called attachment proteins that allow it to recognise, bind to and access certain cell types). For example, in canine distemper, the cells that the virus prefers to invade are the cells of the lymphatic system (lymph nodes, thymus), neurological system and the lining cells of the intestine, respiratory tract, urinary tract, mucous membranes (conjunctiva of the eye and lining of the mouth and nose) and skin. When the distemper virus attaches to the right kind of cell, one of two things may happen:
1) the virus outer membrane fuses with the cell membrane, resulting in the virus capsid and RNA being released into the cytoplasm of the cell OR
2) the cell membrane reaches outwards, surrounding the virus and its envelope in a 'bubble' of cell membrane (the process is termed endocytosis). This bubble gets released into the cell's cytoplasm where the virus envelope fuses with it, resulting in the release of the viral RNA and capsid into the cytoplasm.
Either way, the virus RNA ends up within the cytoplasm of the host cell.
This viral RNA remains in the cytoplasm of the cell (the region of the cell that contains all of 'factories' needed to create cellular proteins and molecules). Using one of its own viral proteins: an enzyme which is not normally present within canine cells (an enzyme called RNA polymerase), the RNA virus starts replicating hundreds of identical copies of its own RNA within the animal cell. This process of Distemper RNA replication is a complicated process that involves several steps which, for the purposes of keeping it simple, we will not go into here (the RNA found in distemper is a special form of RNA termed negative-sense RNA - it needs additional steps to be able to replicate). The virus also uses the 'cell's machinery' (various cell enzymes and cellular organelles contained within the cytoplasm) to get the cell to create hundreds of new capsids and viral proteins. Some of these proteins (the surface attachment proteins of the virus) get secreted onto the surface membrane of the dog cell in readiness for the next stage of the process. The new RNA copies get packaged into the newly created capsids, along with other internal viral elements that the cell body has produced. These creations (basically viruses without their enveloping membranes) attach to the inside of the dog cell membrane and 'bud' out, taking a surrounding coating of dog cell membrane with them. This dog cell membrane becomes the new viral envelope and contains all of the viral surface proteins required to attach to and invade other dog cells. The cell dies as a result of the destruction of its cell membrane by the many evacuating viruses.
This repeated process of virus invasion and cell destruction is what causes disease in the animal. In the case of distemper, because the virus needs to make use of the cells of the lymphoid tissues, brain, lung, gastrointestinal tract, urinary tract, skin and mucous membranes in order to replicate, this is where the cell damage occurs: consequently, most of the clinical signs seen relate to these organs. The more severe symptoms of disease are seen when the immune system fails to respond and large numbers of cells start dying as a result of this viral replication.
4b. Effects on the lymphatic-tissues and bone marrow:
When distemper is initially ingested or inhaled by the dog, it first localizes in the lymphatic tissues of the lungs and throat (tonsils, pharyngeal nodes). The virus replicates in these cells before spreading to other lymphatic tissues throughout the body (spleen, liver, lymph nodes of the abdomen, chest and limbs) and the bone marrow. The distemper viruses replicate for 2-6 days in these tissues, growing to very large numbers of infectious organisms.
The cells of the bone marrow and lymphatic tissues are responsible for creating all of the blood cells (white blood cells, red blood cells and platelets) in the body. The white blood cells fight diseases, the red blood cells carry oxygen around the body and the platelets help to clot the blood. When distemper virus invades and damages these cells, the result can be a reduction in the number of cells (white blood cells such as lymphocytes) available in the body to fight diseases and a reduction in the number of circulating blood platelets (usually the reduction in the number of platelets seen with Distemper is not enough to cause overt bleeding disorders). The reduced number of white blood cells available in the body may make these animals more prone to secondary bacterial and viral diseases.
During this early phase of infection (the first 2-6 days of Distemper), all that might be seen is a dog that seems to be non-specifically off colour. He might be lethargic, inappetent (off food) and he might have a fever. Your vet might detect enlarged lymph nodes, but possibly very little else.
After the virus has replicated to massive numbers within the lymphatic and bone marrow tissues, it distributes throughout the body, settling within the cells of the nervous system, the eye and the cells that line the gastrointestinal tract, urinary tract, uterus, respiratory tract, mucous membranes (gums and conjunctiva) and skin. It is during this second phase of replication (replication within these new sites) at 8-14 days after initial infection that the main clinical signs of distemper are seen. It is also during this time that newly made virus particles are shed from the body, ready to infect other animals.
4c. Effects on the intestine:
The intestine of the dog is lined by a thin layer of cells termed an epithelium (i.e. the gastrointestinal epithelium) or a mucosa. These cells have many roles including:
1) absorption of food nutrients from the intestine into the blood
2) secretion of mucus (which prevents digestive enzymes and acids from harming the intestinal lining)
3) forming a barrier to prevent bacteria from the intestines from entering the intestinal tissues and blood.
Distemper virus replicates in the cells lining the small intestine and, during this viral replication, these cells are destroyed. The cells die and disintegrate and fall away from the intestinal wall, resulting in ulceration and bleeding of the intestines. Without these superficial intestinal epithelial cells to line and protect them, the internal tissues (connective tissues, blood vessels etc) of the intestines are exposed to the chemicals and digestive enzymes of the intestine and also to the natural bacterial populations of the gut (which can be harmful to the body without a protective layer keeping them at bay).
Bleeding and dehydration:
 The death of the cells lining the small intestine results in ulceration and bleeding of the intestinal wall, damage which is compounded by the effect of digestive enzymes and bacterial toxins that can further erode the unprotected areas. The severe, diffuse injury of the intestinal lining results in massive inflammation (infiltration of inflammatory cells and proteins into a region of damage) of the gut. The intestine becomes swollen and paralyzed (unable to move) and a condition called ileus (non-moving gut) occurs, which results in vomiting and an inability to keep any food or fluids down. The ulceration, bleeding and massive inflammatory response that occurs in the intestines results in an enormous loss of water and body-proteins into the intestines: these are lost as diarrhea (which can be bloody, watery or mucussy) and vomit. This loss of fluids and proteins is further compounded by the inability of the animal to keep water or food down (due to vomiting) and by the fact that the nutrient-absorbing cell-lining has been lost (there are no cells left to absorb any of the food or water that does make it to the gut). The result is a massive net loss of body proteins (albumin, in particular) and massive dehydration (loss of water), which, if left untreated, will lead to shock and death.
The death of the cells lining the small intestine results in ulceration and bleeding of the intestinal wall, damage which is compounded by the effect of digestive enzymes and bacterial toxins that can further erode the unprotected areas. The severe, diffuse injury of the intestinal lining results in massive inflammation (infiltration of inflammatory cells and proteins into a region of damage) of the gut. The intestine becomes swollen and paralyzed (unable to move) and a condition called ileus (non-moving gut) occurs, which results in vomiting and an inability to keep any food or fluids down. The ulceration, bleeding and massive inflammatory response that occurs in the intestines results in an enormous loss of water and body-proteins into the intestines: these are lost as diarrhea (which can be bloody, watery or mucussy) and vomit. This loss of fluids and proteins is further compounded by the inability of the animal to keep water or food down (due to vomiting) and by the fact that the nutrient-absorbing cell-lining has been lost (there are no cells left to absorb any of the food or water that does make it to the gut). The result is a massive net loss of body proteins (albumin, in particular) and massive dehydration (loss of water), which, if left untreated, will lead to shock and death.
Bacterial invasion into the blood and tissues:
Ulceration of the intestine and loss of the protective gut-lining-cells and their protective mucus secretions allows bacteria normally present in the gut to enter the intestinal wall and blood stream. These bacterial levels in the small intestine can be very high because the gut is not moving (movement of the gut is a normal mechanism by which excessive populations of bacteria get cleared from intestine through the feces). If the gut does not move, the bacteria can just brew away in the unmoving regions of the gut, their populations expanding to massive levels. Bacterial infection can damage the intestinal wall. Should those bacteria gain entry into the blood (a condition termed bacteremia, septicemia or blood poisoning) severe systemic illness and septic shock can result: the bacteria cause extensive inflammation and damage to the blood vessels and organs (e.g. lung, kidney). This can be fatal.
Bacteria can even become deposited into the small capillaries of the joints, eyes, heart and kidneys, leading to infection and abscesses within these places.
Intussusception:
An additional note: spasming and thickening of the intestine during distemper virus infection can result in the gut telescoping into itself and a complication caused intussusception. Correction of this complication requires surgery: surgery that is likely to be done on an already malnourished, possible septic and compromised animal. Not ideal.
4d. Effects on the respiratory tract and mucous membranes:
The respiratory tract (nasal passages, throat, trachea, small airways and alveoli) of the dog is lined by a thin layer of cells termed an epithelium (i.e. the respiratory epithelium) or a mucosa. These cells have many important roles including:
1) secretion of mucus which captures dust and infectious organisms (bacteria, viruses) and prevents them from reaching the small airways (the important regions deep inside the lungs where oxygen enters the blood).
2) forming a cell barrier to prevent bacteria from the respiratory tract from entering the lung tissues and blood.
3) Some cells have motile hairs on them to move mucus and contaminants out of the lungs and up to the mouth for coughing out or swallowing.
4) transfer of oxygen into the blood.
 When these cells become infected with the distemper virus, they become damaged and degenerate. The resultant ulceration and damage of the lining of respiratory tract leads to severe irritation and inflammation of the affected regions (trachea, throat, lungs and lining of the nose). The irritation causes the animal to cough and sneeze. Large volumes of protein-filled inflammatory fluids and mucous (mucous is produced in larger amounts by respiratory epithelial cells that are irritated as a last ditch effort to remove the invading organisms) floods the respiratory tract. The animal coughs up fluid and may find it hard to breathe particularly if the inflammation involves the thin layers of cells of the deepest regions of the lung, where the oxygen gets transferred into the blood. Severe fluid build up in the lungs (pneumonia) can lead to lack of oxygen entering the bloodstream and death. Severe irritation of the nasal passages can result in a thick, mucoid nasal discharge and sneezing.
When these cells become infected with the distemper virus, they become damaged and degenerate. The resultant ulceration and damage of the lining of respiratory tract leads to severe irritation and inflammation of the affected regions (trachea, throat, lungs and lining of the nose). The irritation causes the animal to cough and sneeze. Large volumes of protein-filled inflammatory fluids and mucous (mucous is produced in larger amounts by respiratory epithelial cells that are irritated as a last ditch effort to remove the invading organisms) floods the respiratory tract. The animal coughs up fluid and may find it hard to breathe particularly if the inflammation involves the thin layers of cells of the deepest regions of the lung, where the oxygen gets transferred into the blood. Severe fluid build up in the lungs (pneumonia) can lead to lack of oxygen entering the bloodstream and death. Severe irritation of the nasal passages can result in a thick, mucoid nasal discharge and sneezing.
Damage to the lining of the respiratory tract also results in an inability of the respiratory tract to get rid of the bacteria that normally inhabit the region. The secretion of mucous becomes excessive, trapping bacteria in the airways, and the motile hairs needed to push the mucus out of the lungs become paralysed. The loss of the barrier epithelial cell layer enables the bacteria to attach to the exposed tissues underneath and the excessive amounts of inflammatory proteins and secretions in the damaged regions feeds the bacteria, allowing their populations to grow. As a result, a secondary bacterial pneumonia (bacteria and pus in the lungs) often occurs following viral lung damage. The added bacterial toxins and pus created can make the animal very sick. Animals with severe pneumonia can die of an inability to get oxygen into their lungs and/or from bacterial invasion of their blood and organs, which can result in multiple organ damage and organ failure.
The respiratory epithelium that lines the lungs is continuous with the mucous membranes lining the eyes, nostrils and mouth (the cells on the surface of gums and conjunctiva of the eyes are mucous membranes too, lined with similar epithelial cells). Viral damage can extend to these regions, resulting in swelling, ulceration and inflammation of the gums, conjunctivae and nasal passages. The animal develops irritation and swelling of the eyes (eye pain, squinting and a watery ocular (eye) discharge), nose (nasal discharge and sneezing) and mouth. Secondary bacterial infection of the nose and eyes can occur, resulting in a secondary, pussy bacterial conjunctivitis and rhinitis (inflammation of the nose).


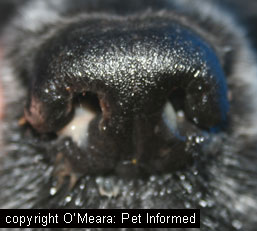
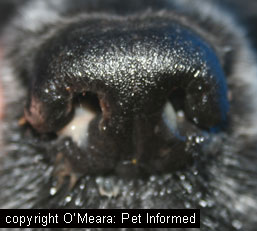
The first image is of the normal mucous membranes (gums) of the mouth.
The second image shows the normal mucous membranes lining the underside of the eyelid (pink) and the surface of the sclera (white of the eye). These are all termed conjunctiva - they are basically a layer of epithelial cells. They are susceptible to damage by diseases such as distemper.
4e. Effects on the nervous system (brain and nerves):
Of all of the organs that distemper can infect (and there are many), distemper is probably most well known for its effects on the brain and nervous system. Animals afflicted with severe, generalized distemper will often have had the gastrointestinal and respiratory signs before the onset of neurological signs begins. They often have started to recover from the gastrointestinal and respiratory signs, through good medical management, before the neurological signs appear (neurological signs tend to appear within 1-3 weeks of the other signs starting to abate). This can be very distressing and disheartening for owners who think that their pet is starting to recover.
Damage to the cells of the nervous system can occur in any part of the brain or the peripheral nerves (nerves of the spinal cord and limbs), sometimes with multiple areas being affected at once. As a result, there is no 'typical' neurological presentation that occurs with distemper. Any nerves can be affected and so the neurological signs of distemper can be varied and bizarre. Puppies may spin their heads around, seizure, fall over, walk drunkenly, stargaze, seem to be deaf or blind, seem paralysed in a leg, seem unable to get up ... anything really. The signs seen will give an indication as to which area(s) of the brain or nervous system are being injured by the virus.
For example:
Injury to the front of the brain (brain hemispheres) - results in circling, fits (seizures), mental depression.
Injury to the cerebellum (back of the brain) - results in wobbliness and tremoring as the animal walks or moves.
Injury to the vestibular region of the brainstem - results in a head tilt, falling and eye-flicking (nystagmus).
Injury to a nerve of a limb - results in knuckling or paralysis or rigidity of a limb.
Of all of the many and varied neurological signs that can be seen, distemper is particularly well known for two in particular:
1) Distemper chorea - termed 'chewing gum seizures' distemper chorea is a rhythmic, repetitive contracting and relaxing of a single muscle group (often the muscles of a limb or the muscles of the jaws - the animal repetitively clenches its teeth and looks like it is chewing gum). The symptom is seen in other disease states, but is most commonly associated with CDV.
2) Old-dog encephalitis - dogs that get distemper, but which do not die (they either recover from severe disease or they fail to develop severe disease due to the presence of some anti-distemper immunity), may have small levels of distemper virus persist for years within their brain tissue. This persistent neuronal distemper can result in a slowly progressive disease that looks like other forms of canine dementia. The animal may seem to become progressively blind and vague and may pace and circle a room endlessly or stand with its head pressed to a wall. These animals may not have any gastrointestinal, respiratory, eye or skin signs and, consequently, are not likely to be infectious to other pets.
The neurological signs seen with distemper will often tend to progress, once started, and there is generally no cure for them. If the neurological signs seen are not considered to be compatible with a good quality of life, these animals may need to be euthanased.

See how the angle of the mouth is dropped down (it should go up, like a smile, in normal dogs)? This nice staffy had paralysis of the facial nerve on both sides of its head, caused by distemper. In addition to being unable to lift its lips, the dog was also unable to blink either eye.
Note that some animals affected with distemper will only show neurological signs. They may not show any sign of respiratory, gastrointestinal, ocular or skin disease at all. Animals that only have neurological signs do not shed distemper and are unlikely to be an infectious risk to other animals.
Important point - Distemper versus rabies:
One thing that is important to note: for those of you who have rabies in your country, many of the neurological signs of rabies can be similar to the neuro symptoms of distemper. Even worse, many of the exact same species of wild animal that are known for carrying rabies (raccoons, skunks, dogs, foxes) can also be afflicted with distemper. It is impossible to tell just from looking at an animal which neurological disease it might have (not all animals with distemper show the gastrointestinal or respiratory symptoms). You can not catch distemper, but you can catch rabies! For your own safety, treat every unvaccinated animal displaying strange neurological signs as a potential rabies case rather than a potential distemper case and take suitable precautions when dealing with them. Call your local authorities for advice.
4f. Effects on the skin:
Similar to the effect of the epithelial cells lining the gut and the respiratory tract, the cells that make up the skin of a dog are just another tough layer of superficial epithelial cells, which line and protect the body and underlying tissues from external injuries and diseases.
Because it likes to infect and damage epithelial cells, canine distemper also tends to infect the outer skin of the dog. This damage results in a number of different skin lesions, the most typical being:
- 'hardpad' - the pads of the feet become excessively thickened.
- 'hardnose' - the nose of the dog becomes excessively thickened and horny.
- pustular dermatitis - some puppies with distemper have pustules (small pimples or zits, similar to acne) over their skin.
- juvenile cellulitis - this can be part of the hypertrophic osteodystrophy (HOD) condition which sometimes occurs with disease-type or vaccine-related distemper. It typically presents as young dogs with fever, inappetence, swelling of the face and limbs and pustules or crusting of the skin. If affected with HOD, these animals will also be lame with painful, swollen legs and joints.


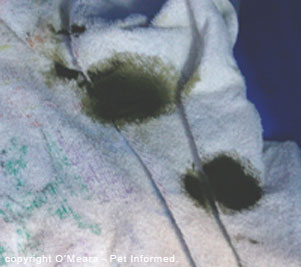
Examples of hardnose and hardpad.
4g. Effects on the eyes:
The eyes of the dog can also be affected by canine distemper virus. As described in the respiratory and mucous membranes section, distemper commonly causes inflammation and infection of the membranes of the eye (the conjunctiva), a condition termed conjunctivitis. This results in pain, redness and weeping (eye discharge) of the eyes.
Occasionally, distemper can cause other eye problems, including:
 - distemper uveitis (inflammation within the eye itself) - the surface of the cornea (clear part of the eye) will become cloudy in appearance; the pupil will shrink to a small size and the sclera (white of the eye) will become inflamed and red. The eye will be painful and the animal will squint. Left untreated, the inflammation within the eye can damage it permanently and secondary complications such as glaucoma may occur that can make the animal permanently blind.
- distemper uveitis (inflammation within the eye itself) - the surface of the cornea (clear part of the eye) will become cloudy in appearance; the pupil will shrink to a small size and the sclera (white of the eye) will become inflamed and red. The eye will be painful and the animal will squint. Left untreated, the inflammation within the eye can damage it permanently and secondary complications such as glaucoma may occur that can make the animal permanently blind.
- optic neuritis - distemper can damage and inflame the optic nerve (nerve which takes information from the retina of the eye to the brain) and the animal may become blind in that eye. Obviously, being a nerve, this condition (optic neuritis) is actually part of the nervous system form of distemper: I have included it under the eye section because the eye effects and blindness are what owners often notice.
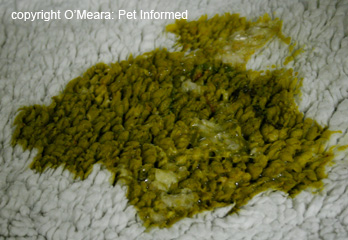
- 'dry eye' (keratoconjunctivitis sicca or KCS) - the distemper afflicted animal can lose the ability to produce tears and this will result in a dry eye that is crusted with thick green to brown mucus. See image. Many of the dogs that get the dry eye symptom of distemper are dogs which have had the disease, but have survived it (they either recovered from the severe disease or they failed to develop severe disease due to the presence of some anti-distemper immunity).
4h. Effects on the joints and bones:
Distemper can affect the joints and bones of a dog. The kinds of joint and bone problems which are most commonly attributable to canine distemper virus include:
1) Hypertrophic Osteodystrophy (HOD) - HOD is a disease which affects the growth plates of young growing dogs, in particular larger breeds such as the Weimaraner and Great Dane. The condition is diagnosed on the basic of distinctive radiographic bone changes and tends to present as lameness, fever, lymph node swelling and bone pain. Occasionally HOD cases present with concurrent skin disease: skin swelling and pussy skin infections; a condition termed juvenile cellulitis. Distemper and distemper vaccines are considered to be among the major causes of the HOD condition, but host factors are also thought to play a big role (e.g. Weimaraners are thought to be susceptible to live vaccines due to an inherent immune suppressive condition within the breed-lines).
2) Rheumatoid arthritis - Rheumatoid arthritis is an immune mediated condition where immune complexes (viral antigens bound with the body's immune antibodies) get deposited in the joints of the animal. These immune complexes get attacked by the cells of the immune system and, during the severe inflammatory reaction that results, the joints can become badly inflamed, swollen and damaged. There are many causes of rheumatoid arthritis and CDV is just one of them.

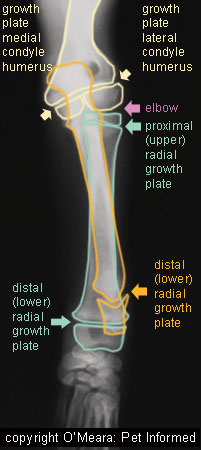
Correction - the description: "distal radial growth plate" written in orange lettering, should read "distal ulna growth plate." Sorry for the confusion.
Effects on other parts of the body:
Distemper can also have effects on other regions of the body. It can affect the unborn fetuses of pregnant bitches, causing these puppies to either die in utero, be aborted or be born alive, but with progressive neurological disease, permanent immune suppression or progressive wasting disease (puppies that grow weaker and waste away after birth are termed fading puppies: there is many causes for this and distemper is but one of them). Distemper can affect the developing permanent teeth of young animals, causing the enamel not to form properly. On occasion, the virus has also been known to affect the heart muscle, resulting in cardiomyopathy, signs of heart failure and even death. Inflammation of the testicles can occur, which may reduce fertility and testosterone levels in male dogs.
4i. Minimal or absent clinical signs:
Not all animals affected with distemper virus will progress to the severe, generalised and often fatal disease symptoms described in the previous section 4 subsections. Instead, animals may sometimes show no signs of disease or only very mild signs of disease.
Carriers - animals with no clinical signs:
It is possible for some dogs (and puppies) that have been fully vaccine-protected or which have achieved partial vaccine protection to be exposed to distemper and to replicate the virus temporarily in their bodies. Some of these animals will replicate virus in and shed the virus from their bodies, but show no signs at all. These animals are termed carriers and they are a significant infectious disease risk to other, unprotected animals because they shed infectious viral particles without anyone being aware that they have the disease. This virus shedding can potentially occur for up to 3 months following infection. Carriers are thought to be very common among the dog population (more common than severely affected animals), but they usually go undetected and so the real incidence of carrier numbers is often uncertain.
Animals with mild clinical signs of distemper:
Some animals infected with distemper may develop mild gastrointestinal or respiratory signs. These mildly affected animals rarely progress to the severe, usually fatal, generalised disease symptoms seen in distemper of unvaccinated puppies and dogs and they will often recover quickly with a minimum of medical intervention. Much of the time, these mild disease signs often go undiagnosed as distemper because they mimic a large range of other, more common, self-limiting diseases (e.g. kennel cough). During their period of mild illness, and in the months following infection (potentially up to 3 months), these animals will shed infectious distemper particles into the environment, which could pose a risk to the under vaccinated.
Note - it is possible for these apparently 'recovered' animals to retain low levels of distemper in their bodies (especially the brain) for many years. These animals might possibly go on to develop distemper-related diseases such as chronic, progressive dementia (old dog encephalitis) in the years to come.
When do distemper animals get the severe signs and when do they get the mild signs?
Whether or not the animal develops only mild (or absent) clinical signs or progresses to severe, life-threatening symptoms depends directly on the degree of immune protection the animal possesses. Animals with absent or very low antibody titers tend to develop severe, generalised, progressive disease signs. These animals tend to be unvaccinated animals, inappropriately vaccinated animals, immune suppressed animals and young puppies that did not receive their colostrum (maternal immunity). Animals that develop only mild signs (or no signs) of disease tend to have some level of protective antibody in their blood.
4j. Disease caused by live distemper vaccines:
Some strains of live distemper virus are relatively virulent and, under certain conditions, are capable of causing disease symptoms somewhat similar to those seen in the wild-type, environmental distemper condition. Generally, disease caused by distemper vaccination is very rare. We tend to only see it in three main situations:
1) When live distemper vaccines are given to animals which should not receive them - e.g. when distemper vaccines are given to pregnant bitches, underage puppies, immune suppressed animals (e.g. pets on chemotherapy) or to sick animals harbouring other diseases, such as parvovirus.
2) When certain vaccine strains are administered to susceptible animals - e.g. according to textbooks (e.g. Greene CE), the Rockborn strains and Snyder Hill strains of distemper vaccine are more likely to cause problems of virulence and disease than the Onderstepoort strain or recombinant distemper vaccine is.
3) When certain susceptible breeds and lines of dog (e.g. certain lines of Weimaraners), thought to have a poorer immune system, are given certain strains of live distemper vaccine.
Vaccine-related distemper signs can include:
HOD (hypertrophic osteodystrophy).
As discussed in section 4h., HOD is a disease of the growth plates of young, growing bones. Typically occurring in large breed dogs (Weimaraners, great danes) of around 3-6 months of age, HOD is a very painful condition characterized by lameness, fever, bone pain and joint swelling. Occasionally, juvenile cellulitis (a skin disease) and gastrointestinal symptoms will occur in addition to the HOD. The vaccine-associated condition usually occurs within 3 weeks of distemper vaccination (Rockborn and Snyder Hill strains tend to be most commonly associated, though all live vaccines can do it). Treatment for the condition is generally symptomatic. Pain relief and steroidal anti-inflammatories (non-steroidals can be ineffective) are usually required to treat the condition and the condition generally takes up to 6 weeks to resolve (longer if prompt treatment is not instigated).
Severe acute neurological disease (clinical distemper of the brain).
Infection of the brain (encephalitis) can occur in animals vaccinated with certain strains of distemper vaccine (Rockborn and Snyder Hill strains tend to be most commonly associated with neurological symptoms). Generally, vaccine-associated neurological disease only occurs in immune suppressed animals; in puppies of bitches vaccinated during pregnancy; in puppies vaccinated while underage (under 4 weeks) and in animals vaccinated with live vaccines whilst infected concurrently with another disease (e.g. parvo). Similar to the neurological condition that occurs with true distemper, the region of the brain affected with canine distemper vaccine can be very variable, as can the symptoms which result. Animals can have any number of neurological signs, including fits, wobbliness, distemper chorea and paralysis. Similar to the neurological condition which occurs with wild-type distemper, the neurological signs of vaccine-associated distemper can be progressive and fatal, although, typically, vets have a better chance of ceasing and improving the neurological condition of an animal with this condition that they do with a true distemper infection.
Chronic progressive neurological disease.
Distemper vaccines can induce a slowly, progressive neurological disease which appears similar to other forms of canine dementia.
Infection of the fetuses.
Vaccination of a pregnant bitch with a live vaccine can result in still-birth and abortions of puppies. Puppies can also be born alive, but with progressive neurological symptoms; severe immunosuppression or 'fading puppy syndrome' (a condition with many causes, where puppies that are born weak and stunted and lethargic and simply waste away and die). For more on vaccinating pregnant bitches, click here.
Reduced blood platelet counts.
Live distemper vaccines can reduce blood platelet counts in animals. These reduced platelet counts are generally not severe enough to cause overt bleeding.
Distemper vaccines can cause other side effects (allergies etc.) too, side effects that can occur with any vaccine type. For more info on general vaccine side effects, click here.

5. Diagnosis of canine distemper - how do we test for distemper?
Distemper can be one of the more difficult conditions to diagnose in the live animal. Often animals with severe distemper are presumptively diagnosed on the basis of their clinical signs, history (e.g. age, absence of vaccination) and their progressive neurological symptoms, which are non-responsive to medical management. Euthanasia of severely infected animals invariably results and definitive diagnosis is usually achieved from examination of tissue samples taken at post-mortem.
5a. Blood tests - general blood panel:
The changes seen on general blood analysis of a distemper dog tend to be very non-specific and not diagnostic of distemper. Changes include a low lymphocyte count (a lymphocyte is a type of white blood cell) and a reduced platelet count. Sometimes reduced levels of blood proteins (albumin and globulins) can occur, but this is not specific for distemper.
5b. Blood testing - virus inclusions:
When distemper first enters the body, it replicates in the cells of the bone marrow and lymphatic tissues, which are responsible for creating all of the blood cell lines (red blood cells, white blood cells and platelets). Sometimes, during this process of cell creation, these viral particles end up inside the blood cells (red blood cells and white blood cells mostly) that circulate in the body. It is, therefore, sometimes possible to see these viral particles on a routine blood smear. The replicating virus particles cluster together in the cytoplasm, forming a visibly-staining patch of viral material called an inclusion or inclusion body.
5c. Blood testing - distemper antibody titres:
Antibodies are protective immune proteins made by certain cells of immune system to attack infecting viruses and other foreign invaders (for details on how antibodies are made and what they do, see our How Vaccines Work page). Each individual antibody protein made is very specific and will only target and attack a particular invading organism. For example: antibodies made against the distemper organism will only attack that organism, no others.
Additionally, it must be mentioned that antibodies are only created in response to the presence of the organism that they are specific to (whether it be the real, wild-type organism or a closely-related vaccine virus organism). Put basically, if an animal is never exposed to distemper or distemper vaccine, the levels of protective, distemper-specific antibodies will be very low. It is only after actual, intra-body exposure to the distemper organism that levels of antibodies increase. This is the purpose of vaccination - exposing the animal to a safe form of distemper so that its immune cells will create protective antibodies.
Distemper antibody levels in the animal's blood can be used as ones means of diagnosing distemper infection. If the animal has never been vaccinated, then, theoretically, its distemper antibody titres should be low. If that same, unvaccinated animal is sick and displays clinical signs of distemper and the antibody levels are high (an unexpected result in an unvaccinated animal), then this might be indicative of active distemper infection and thus diagnostic.
The problem with antibody testing - false positives:
The problem with the above test is that antibodies, once made, last a long time in the body (potentially a year or longer). Therefore, any animal that has been previously vaccinated (even a single vaccine); previously exposed to the virus in the environment or that has maternal antibodies from the mother (very young puppies) will have antibodies against distemper in the blood. These levels can be high and, in the case of a vaccinated or virally-exposed animal, they can last for years. If you were to test such an animal for distemper, because it had suspect symptoms, you would find a high distemper antibody titre. This would not, however, mean that the animal actually had distemper. Even if that animal was well, it would have high distemper antibody levels simply as a side effect of past exposure.
So how do we get around this issue of antibody false positives?
There are two ways that blood antibody levels can still be of some use in helping us diagnose distemper.
The first is that we could measure a short-lived distemper antibody called IgM.
When a body first experiences an invading organism that it has never seen before, it makes antibodies of a specific, short-lasting form called IgM antibodies. Later, as the disease progresses or persists within the body or as the animal is exposed repeatedly to the organism (e.g. repeated viral exposure occurs with repeat vaccinations), the IgM form of the antibody gets replaced by a more persistent, longer lasting form of antibody molecule called an IgG molecule. IgG, because it lasts so long, is not a particularly useful indicator of current infection. IgM, however, is a more useful indicator of current distemper infection because it is the form of antibody made when an animal is first exposed to a new pathogen: high distemper IgM antibody levels are more suggestive of recent, active infection.
The second is that we could repeatedly measure antibody titres over time.
Over time and, with a lack of repeated exposure to a particular organism (e.g. an animal that did not get booster vaccines), the levels of the longer-lasting IgG antibodies in the blood will decline. When the body is finally re-exposed to the organism (for example an animal that got its booster or was exposed to distemper in the environment) the immune system cells fire up and start making lots of IgG antibodies. (IgM is mostly made with the very first exposure to an organism, not with repeat exposures as described here). Consequently, measuring distemper IgG levels over several weeks can indicate active infection. If the levels are acutely increasing by large amounts (four-fold increase over 2-3 weeks), this could be indicative of recent, active infection.
Animals with very slow, long term, progressive distemper disease (e.g. old dog encephalitis) are unlikely to have high IgM or a noticeable acute rise in IgG (because the disease is so insidious and gradual). All you will see is high-level IgG, but it won't be possible to tell if this is due to currently active disease or due to previous exposure by the disease or a vaccine. Thus, blood antibody levels are not especially helpful in determining if a long-term chronic case is a distemper case.
5d. CSF (cerebrospinal fluid) and/or ocular fluid antibody levels:
Testing distemper antibody levels in the brain fluid (CSF) or eye fluid (termed aqueous humor) of an animal showing neurological or ocular (eye) signs of distemper is probably one of the more accurate tests of distemper available to us.
The brain and the eye are two spaces in the body that are relatively isolated from the general blood circulation of the body (there are cellular barriers between the general blood circulation and the tissues of the eye and brain - this natural barrier is to stop toxins and infections of the body from easily accessing the eye or brain). When distemper invades the enclosed environment of the brain or eye, it gets attacked by immune system cells present within those spaces. These cells make antibodies against the distemper. Consequently, the levels of antibodies in the brain fluid or the eye fluid rise to large levels very quickly. Because of the natural barrier that exists between the brain or eye fluid and the rest of the bloodstream, however, these antibodies are not able to easily enter the main blood stream. What you will see, therefore, in active, recent eye or brain infection, is a high level of distemper antibody in the brain or eye fluid and a comparatively lower level of distemper antibody in the blood.
Testing procedure 1:
The veterinarian takes a blood sample and then he either takes a sample of fluid from inside the eye (in animals with signs of internal eye inflammation) or a sample of CSF fluid from the spinal canal (in animals with neurological signs).
The level of distemper antibody is measured in both the blood sample and in the eye or brain fluid sample.
If the level of antibody in the eye or brain fluid is much greater than the levels of antibody present in the blood - this is indicative of recent, active distemper infection.
Note - there are some inaccuracies with this technique if there has been leakage of antibodies into the CSF from the blood (for example if blood was able to contaminate the eye or brain fluid during the sampling procedure). In order to rule out this potential source of error, testing procedure 2 is preferred and will likely give more accurate results.
Testing procedure 2:
The veterinarian takes a blood sample and then he either takes a sample of fluid from inside the eye (in animals with signs of internal eye inflammation) or a sample of CSF fluid from the spinal canal (in animals with neurological signs).
The level of distemper antibody is measured in both the blood sample and in the eye or brain fluid sample and the ratio of fluid:blood distemper antibody calculated.
The level of antibodies for a different disease (e.g. usually parvovirus antibody) is measured in both the blood sample and in the eye or brain fluid sample. The ratio of fluid:blood parvo antibody is calculated. The parvo antibody testing must be performed using the same measuring techniques as for the distemper antibodies.
If the ratio of fluid:blood distemper antibody is much greater than the ratio of fluid:blood parvo antibody, then this is indicative of active distemper infection.
Technique 2 is more accurate because it enables vets to rule out whether there has been contamination of the eye or brain fluid sample with blood. If there has been blood contamination, then parvo antibodies would also be expected to leak into the fluid samples along with the distemper antibodies and thus the ratios would be expected to be similar.
If the distemper animal does not have eye or brain disease, then local antibodies are unlikely to be produced and this test may yield a false negative result for the disease.
It is important to note that taking fluid samples from the eye or brain (termed a CSF tap) is not innocuous. Withdrawing fluid from the eye carries with it the risk of bleeding within the eye; introducing infection into the eye and even permanent damage to the eye and loss of sight. Withdrawing fluid (CSF) from the brain carries with it the risk of introducing infection into the spinal canal; the risk of permanent spinal cord injury and the risk of the brain herniating out of the skull (if brain pressure is high). These procedures should only be attempted by veterinarians experienced in the techniques.
5e. Cerebrospinal fluid analysis:
Assessment of the numbers and kinds of white blood cells and proteins present in the cerebrospinal fluid can also be useful in the diagnosis of distemper. Typically, the CSF taken from animals with neurological distemper will contain higher than normal CSF protein levels and high numbers of lymphocytes (one of the kinds of white blood cell present in the body). Occasionally, distemper virus inclusion bodies (see section 5b) will be seen in CSF cells.
These cell and protein changes are not definitive for distemper but, when considered along with the animal's presenting signs and history, they can provide added 'evidence' for a distemper diagnosis.
If distemper of the brain is very early or if the distemper has not infected the brain at all, the CSF may be relatively normal in appearance and therefore of no help diagnostically.
5f. Tissue samples - fluorescent antibody testing:
Because distemper invades the cells of various organs in order to replicate, it is possible to detect and visualize (by means of special stains) the organism in affected tissue samples taken from animals that are sick or that have succumbed from the disease (samples taken at post mortem). Tissues that are of value are the tissues that the organism routinely infects. These include lymph node samples, tonsil samples, conjunctiva samples, spleen samples, CSF cell samples, brain, bone marrow samples, skin samples, footpad samples, respiratory and gastrointestinal epithelium samples.
How does tissue testing for distemper work?
 As mentioned in section 4a, the distemper virus has certain proteins and molecules present on its surface membrane (envelope) which allow it to attach-to and invade certain cells of the animal body. These surface proteins/molecules are not only present on the membrane of the virus itself, but they are also secreted onto the surface of any dog cell membrane that happens to be invaded by the virus. These surface proteins and molecules (termed antigens) of the distemper virus are the regions of the virus that are targeted by distemper-specific antibodies of the canine immune system. For a great explanation of antibodies: how they are created and what they do, visit our How Vaccination Works page.
As mentioned in section 4a, the distemper virus has certain proteins and molecules present on its surface membrane (envelope) which allow it to attach-to and invade certain cells of the animal body. These surface proteins/molecules are not only present on the membrane of the virus itself, but they are also secreted onto the surface of any dog cell membrane that happens to be invaded by the virus. These surface proteins and molecules (termed antigens) of the distemper virus are the regions of the virus that are targeted by distemper-specific antibodies of the canine immune system. For a great explanation of antibodies: how they are created and what they do, visit our How Vaccination Works page.
This ability of distemper antibodies to bind specifically to distemper antigens is what is taken advantage of when testing tissues for the presence of distemper. Tissue sections taken from dogs thought to be infected with distemper are exposed to a solution of anti-distemper antibodies which have been bound to a special fluorescent dye. If distemper antigens are present within or on the surface of the animal tissue cells, the antibody/dye complexes will bind to the antigens on the tissues. Under special lighting, distemper-positive cells which have bound the antibody/dye complexes will fluoresce (the dye bound to the antibody is the part that fluoresces), making the affected cells easy for scientists to spot under a microscope.
Can a dog test negative for distemper with this test and still have the disease?
Yes. Such results are termed false negative results and they can occur for two main reasons:
1. The wrong (unaffected) tissue was sampled.
Distemper does not affect all of its favoured cell-types in the body in all animals or at all times. For example: some animals might present with only respiratory signs and never show any brain signs and, as a result, samples of their respiratory tissues might show up positive for the test, whereas CSF or brain tissue might come up negative. Brain tissue would be negative for distemper, but the animal itself would be positive. Another classic example is seen in the tissues of the lymphatic system and bone marrow. These tissues are the ones which are first affected by distemper (the first 2-8 days) and, if testing is performed on these tissues in the first week of infection, they will most likely come up positive. As the disease progresses, however, the animal's own antibodies will start to remove the virus from these initially affected tissues (by this stage, the virus will have spread to other, new tissue sites) and they will start to test negative using this antibody test.
Note - virus tends to persist for longer in some tissues (eye, footpad, skin) and so sampling from lesions in these regions may be more valuable.
2. Interference by the animal's own antibodies as the disease progresses.
As the disease progresses over time, the animal's own immune system will start to respond to the presence of the invading organism: the immune system will mobilise defensive cells and produce its own anti-distemper antibodies to try to kill the virus. These self-made antibodies will bind to viral antigens in the tissues and this attachment will potentially 'block' the antibody/dye complexes in the distemper test from getting exposure to the antigens. The inability to the antibody/dye complexes to bind to the affected tissues will result in a false negative result.
5g. Up and coming tests: PCR and virus culture:
Advancements in viral genetics studies and in the fields of DNA and RNA mapping have enabled scientists to design tests which are capable of detecting tiny amounts of viral RNA or DNA contained in tissue and cell samples using PCR. PCR is a very sensitive testing technique and the presence of distemper RNA in a tissue sample is highly supportive of infection with this organism. At present, distemper PCR is available, but very few labs are equipped to do it commercially. As PCR technology expands, this will most likely be one of the distemper tests of the future.
Virus culture: culturing viruses from tissue samples using specially grown tissue cell lines, is another technology that is also moving ahead in leaps and bounds. Certain labs are able to culture distemper virus from tissue samples affected with the organism. Culturing large amounts of virus allows the virus to be readily identified.

6. Canine distemper treatment.
 There is no easy remedy or cure for distemper virus. No antiviral medication has yet been produced or made available in any mainstream capacity that will kill this organism. Consequently, the treatment of canine distemper infection is pretty much a treatment of symptoms. The aim of therapy is to keep the animal stable, and to manage and prevent any secondary complications, in the hope that the animal's own immune response will take over and destroy the disease before it does any irreversible damage (e.g. severe brain damage). The treatment options for distempervirus, their mechanisms of action and their pros and cons are discussed below.
There is no easy remedy or cure for distemper virus. No antiviral medication has yet been produced or made available in any mainstream capacity that will kill this organism. Consequently, the treatment of canine distemper infection is pretty much a treatment of symptoms. The aim of therapy is to keep the animal stable, and to manage and prevent any secondary complications, in the hope that the animal's own immune response will take over and destroy the disease before it does any irreversible damage (e.g. severe brain damage). The treatment options for distempervirus, their mechanisms of action and their pros and cons are discussed below.
An important thing to remember with distemper, before having your vet undertake any treatment, is that distemper of the nervous system (brain) is usually progressive, and carries a very poor prognosis (depending on the type of neurological symptom seen and whether it is compatible with life). Even more frustratingly, these neurological signs of distemper can often develop after the other signs have resolved. What this means is that, after expending all of that money and emotion (you'll shed a lot of tears) on therapy, your beloved puppy, who seemed to finally be improving, may suddenly deteriorate neurologically and irreversibly.
1) Intravenous fluids.
Animals with severe vomiting and diarrhea which are pouring massive amounts of inflammatory and intestinal-secretory fluid out into their bowels, can dehydrate very fast. Puppies with severe gastrointestinal signs of distemper almost always need some degree of intravenous fluid support.
Sometimes, distemper affected puppies can become so collapsed and dehydrated (severe shock signs) that the veterinarian can't get an intravenous catheter into them in order to give them the essential life-saving fluids. In these cases, the vet will sometimes put a catheter into the puppy's jugular (large vein in the neck) or place a needle inside the bone of the thigh (femur) or upper foreleg (humerus) to administer fluids. Don't be alarmed to see your vet do this: these are perfectly acceptable ways of giving fluids to young animals which are in severe shock.
Often the vomiting and diarrhea is associated with a severe loss of blood salts (called electrolytes) into the intestines. Abnormal electrolytes can lead to weakness, neurological signs, heart arrhythmias and even death and so it is important that their levels are replaced. This can be achieved by placing electrolyte replacers into the fluids that are administered to the puppy. Glucose levels can also become very low in puppies with distemper (glucose is used up by multiplying bacteria and by the inflammatory cells that come in to treat disease) and so glucose will need to be added to the fluids to keep the levels normal.

2) Antibiotics.
Animals with gastrointestinal ulceration and damage to their respiratory tract cellular linings are at huge risk of developing overwhelming infection from secondary bacteria which can invade the ulcerated regions and enter the blood stream. In particular, it is not uncommon for pets with distemper to develop severe pneumonia. This issue of infection is further compounded by the fact that, in distemper, some of the animal's white blood cell lines are reduced: this reduces the animal's ability to fight infection. Broad spectrum, bactericidal (antibiotics that actually kill bacteria, not just suppress them) intravenous antibiotics are a key element of distemper virus treatment.
Commonly used antibiotics include:
Intravenous third generation cephalosporins.
Intravenous ticarcillin/clavulanic acid (e.g. Timentin).
Intravenous fluoroquinolones (e.g. enrofloxacin (Baytril), ciprofloxacin).
Note that these medicines are considered contraindicated in pups under 12 months old (18 months for big breeds) because of the effects of these drugs on growing bone cartilage. If these pups are really sick, however, it may be vital to use these 'contraindicated' antibiotics if we are to save them. Another thing to mention about these antibiotics is that they can, in some cases, cause the animal to display neurological signs. It is important to remember that neurological symptoms can be a side effect of the fluoroquinolone drugs and that the presence of neurologcal signs is not always an indicator of distemper virus invading the brain.
Intravenous aminoglycosides (e.g. gentamicin).
This family of antibiotic drugs is known to be toxic to the kidneys and therefore should not be administered to dehydrated animals (i.e good hydration needs to be achieved first). These antibiotics are also known to be less toxic if given as a higher, once-a-day dose than as a lower, many-times-a-day dose.
Intravenous metronidazole.
Similar to the situation described with the fluoroquinolones, it is possible for this antibiotic medication to cause the animal to display neurological signs. It must be remembered that antibiotics could be a cause of neurological symptoms (these symptoms carry a good prognosis for recovery if the drug is discontinued), not just distemper virus invading the brain (distemper of the brain carries a very bad prognosis).
Tetracyclines (e.g. doxycycline).
These antibiotics are often used in various combinations to achieve broad spectrum. Timentin with enrofloxacin is a nice-broad spectrum combination, as is Timentin with gentamicin.

3) Anti-emetics (drugs that stop dogs vomiting).
Anti-emetic drugs are often used to make puppies feel better (it must be terrible vomiting all the time), to reduce the loss of fluids through repeated vomiting and to get the gut moving again (many work by making the intestines mobile again).
They are best given as continuous rate infusions (i.e. given in a constantly-running drip) rather than frequent injections.
4) Anticonvulsant medications.
Animals with distemper of the brain can present with repeated, uncontrollable seizuring. In an attempt to control these fits, which can cause worsening brain injury if allowed to persist, anticonvulsant medications may need to be administered.
The most commonly administered anticonvulsant medications are the benzodiazepine drugs: diazepam (Valium or Pamlin is the trade name) and midazolam (Hypnovel). These are given intravenously in the form of injections or continuous intravenous infusions. The drugs are powerful anticonvulsants, good for controlling acute seizures, but they do not last long, often wearing off after 30-60 minutes or even less. These drugs are not practical for seizure-preventative usage outside of the veterinary clinic system.
In addition to the benzodiazepine drugs are the barbiturates: phenobarbitone and pentobarbitone (nembutal). These are longer-lasting, powerful anti-convulsants which can be used in the hospital (in tablet and injectable form) and also in the home (in injectable form).
What must be mentioned here, however, is that, in the case of distemper disease, by the time your pet has developed enough neurological signs to require the repeated usage of anticonvulsant medications, it may be too late to save him or her. Distemper cases with severe neurological disease usually die and anti-convulsant medications may only be able to abate the signs for a limited period of time.
Dogs with infrequent fits may be able to go home eventually. These animals are often managed similarly to those with epilepsy and placed on various long-term drugs such as phenobarbitone tablets (e.g. Epiphen, Phenomav, Phenobarb) and potassium bromide tablets (e.g. Epibrom).

5) Anti-inflammatory medications.
Anti-inflammatory corticosteroid drugs (prednisolone, dexamethasone) are often trialled in animals with severe, progressive neurological signs in an attempt to control brain inflammation and swelling and reduce the deteriorating neurological symptoms. The drugs often have some, limited effect and the animal may even appear to improve marginally. Sadly, these improvements are all-too-often transient and the neurological decline may continue to progress.
Note that corticosteroids are not ideal for dehydrated animals or animals with severe intestinal ulceration because they can cause kidney damage and worsening of gastric ulceration. These drugs also cause some degree of immune suppression (they reduce white blood cell numbers and effectiveness), which means that they have the potential to make infectious viral and bacterial conditions worse! On the flip side, they are one of the more powerful brain anti-inflammatory drugs ... basically, the task lies with the veterinarian to determine which of the dog's clinical problems is the more pressing.
Corticosteroids are also often administered to animals with distemper-associated HOD or rheumatoid arthritis in an attempt to resolve the symptoms.

6) Oxygen support.
Animals with viral and/or bacterial pneumonia and inflammatory fluid accumulations within the airways of the lungs can often find it difficult to get enough oxygen into their bodies when breathing normal air. Providing air that is enriched with oxygen can help to improve oxygen delivery to animal's tissues and support the animal while the lung condition resolves itself.
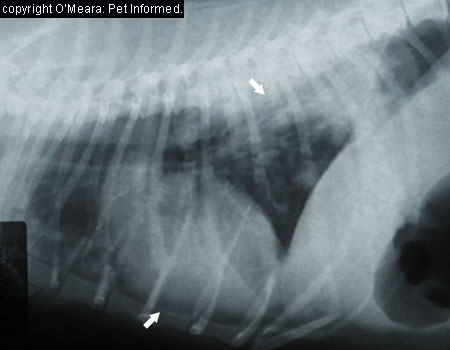
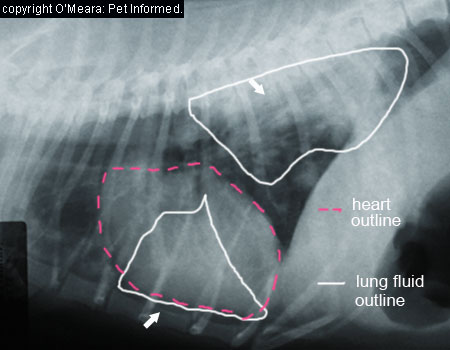
Ways of providing oxygen to animals includes:
1) nasal oxygen tubes - a tube up the nostril delivering oxygen into the throat region.
2) oxygen hood - placing an Elizabethan collar on the animal; covering the openings with glad wrap and putting an oxygen-delivery tube into the enclosed space to deliver a higher level of oxygen to the animal's facial region.
3) oxygen box - placing a small animal into an enclosed cage or humidicrib and pumping oxygen into it.
4) ventilatory support - severely affected animals may not be able to maintain oxygen levels even with nasal tubes and oxygen boxes etc. Some of these animals may require intubation and ventilation to keep their oxygen up. Animals with pneumonia severe enough to require prolonged intubation and ventilation will be very expensive to treat and do carry a very guarded prognosis.

7) Pain relief.
Severe ulceration of the gut and abdominal pain is one of the many distemper symptoms that must be managed. Pain relief must be given to these puppies to make them more comfortable. In addition, those dogs presenting with distemper-associated HOD and rheumatoid arthritis often have severe bone and joint pain and they normally require some degree of pain relief to make them more comfortable.
Generally injectable, opiate drugs (e.g. methadone, fentanyl) are used in these animals to achieve pain control. Oral medications are not kept down. Drugs such as non-steroidals (e.g. carprofen, meloxicam, tolfedine) and corticosteroids (prednisolone, dexamethasone, triamcinolone) are contraindicated in animals with severe, ulcerative intestinal disease.
Because the intestines of these puppies may not move too well (due to ileus), their stomachs can fill with large amounts of fluid. This bloating and abdominal distension is painful. Simply passing a tube into the puppy's stomach (via the mouth) to release the fluid can relieve this discomfort.
Skin scalding around the anus of puppies with diarrhea is also very painful. The scalding can be reduced by applying waterproof, soothing creams to the perineal skin (skin around and under the anus). Useful creams include vasoline (petroleum jelly) etc.
Ulcer medications (next section) can also act to soothe the pain of intestinal ulceration.
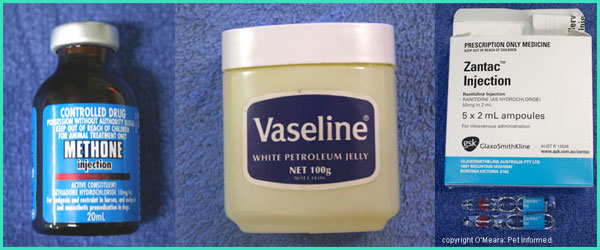
8) Ulcer medications:
Injectable medications are often used to reduce gastric acid production by the stomach in order to reduce the pain of these acids burning on the ulcerated intestine. They have limited effect, but are useful.
Of those that are readily available in most clinics as part of gastrointestinal distemper treatment, intravenous omeprazole is probably the most effective (it is costly, though), followed by the H2-blockers (ranitidine and cimetidine).
Oral antacids and ulcer-coating drugs can be given to animals that can tolerate oral medications (e.g. carafate).
9) Warmth or cooling:
Depending on what is happening with the animal at the time (what symptoms it is presenting with), an animal afflicted with distemper can present to a veterinarian in a cold or overheated state. These animals will need appropriate warming or cooling techniques to normalize their body temperatures.
Warming animals:
Animals that are cold or in shock require warming to normalise their body temperatures. Provision of warmth may be as simple as providing the puppy with warm bedding or a heat pad or it may require extra measures, such as warming the fluid lines, bubble-wrapping the feet and using specialized warming equipment, such as the bear-hugger.

Cooling overheated animals:
Animals that have been seizuring or that have very high fevers or muscle tremors may have excessively high temperatures. These animals may require cooling. This can be done through the administration of cooled intravenous fluids, wetting the body, cool fans, evaporative cooling (placing alcohol in the armpit, belly and groin regions) and cool water enemas.

10) Vitamins?
Water soluble vitamins such as vitamins B and C are lost from the body when animals that are not eating are placed on intravenous fluids (the fluids are eliminated through the kidneys via the urine, taking lots of water soluble salts and vitamins with them). The loss of vitamins (esp. vitamin B) from the body is not ideal for the brain (the brain needs B vitamins) and also acts to suppress the appetite. It can be helpful to give these inappetent animals some B and C vitamins to replace those being lost from the body.
Vitamin C, in particular, used to be advocated for the treatment of HOD (hypertrophic osteodystrophy) in dogs. Its effectiveness in aiding the treatment of distemper related disease is not proven, but giving vitamin C to these animals certainly won't hurt them and could be worth a try.
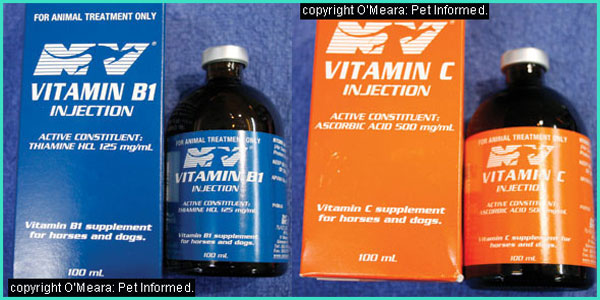
11) Environmental management for home care patients.
 Animals which recover from distemper to the point of being able to go home may have persistent issues (such as blindness or intermittent seizures) which require you to implement an environmental control strategies within your own house. Blind animals, for example, will usually be able to get around fine with time, so long as you take care not to move your furniture around (they end up navigating by smell and by memory); keep clutter out of their way and keep them from accessing places where they might fall and hurt themselves (steps, pools, holes etc). Animals prone to intermittent seizures should, likewise, be kept away from places where they might hurt themselves, should a fit occur. Swimming pools, steps, high verandahs and balconies are probably the biggest risks.
Animals which recover from distemper to the point of being able to go home may have persistent issues (such as blindness or intermittent seizures) which require you to implement an environmental control strategies within your own house. Blind animals, for example, will usually be able to get around fine with time, so long as you take care not to move your furniture around (they end up navigating by smell and by memory); keep clutter out of their way and keep them from accessing places where they might fall and hurt themselves (steps, pools, holes etc). Animals prone to intermittent seizures should, likewise, be kept away from places where they might hurt themselves, should a fit occur. Swimming pools, steps, high verandahs and balconies are probably the biggest risks.
12) Euthanasia:
Distemper that progresses enough to severely affect multiple organs of the body, particularly the brain, carries a poor prognosis and, especially in the case of severe distemper brain disease, may not be curable. Euthanasia is a common and perfectly acceptable option here.
Note - I do not want to give the false impression that all dogs with distemper brain disease need to be euthanased immediately. Not all dogs with persistent neurological disease need to be put down. Some neurological disabilities might look bizarre (e.g. distemper chorea, earlier stages of old dog encephalitis) or seem scary to their owners (occasional, intermittent seizures, blindness), but many of them are manageable (sometimes with the assistance of drugs) for the intermediate or long term.
Monitoring:
Monitoring a severely-affected, septic distemper puppy involves an extremely high level of intensive care work. These animals are about as ill as you can get and their status can change hour to hour: ideally these puppies need 24 hour attention.
Monitoring of these pets varies according to the equipment and expertise of the vets and according to the status and severity of the puppy, but generally it includes:
- regular examinations - checking heart rate, lung sounds, temperature etc.
- regular care of IV lines and catheters
- regular blood pressure and oxygen-level measurements.
- urine monitoring.
- seizure monitoring
- regular treatments (those listed above) and treatment adjustments and
- regular blood testing.
During their stay in hospital, distemper puppies often require lots of blood testing to monitor their levels of hydration, electrolytes, glucose, proteins, oxygen levels, red and white blood cells and organ function. Many of these tests will be performed several times a day and treatment and prognosis adjusted according to the results gathered. Trends over time (a series of measures) are particularly helpful as they can give veterinarians and their owners some idea of prognosis.

The trouble with such intensive monitoring is that, not only does the poor puppy have to get bled several times a day to get the samples, but the repeated lab-work is also expensive for their owners. In the case of severe, generalised distemper, which carries such a poor prognosis, going to this degree of treatment and expense may not be a rewarding use of your finances and it may be putting a terminally ill puppy through a lot of extra pain and suffering.

7. What is the prognosis for Canine Distemper?
Canine distemper is one of more severe infectious disease conditions that can affect an animal. In the case of generalised distemper (that severely affecting multiple organs of the body all at once), the prognosis is normally very poor.
Severe pneumonia and gastrointestinal disease often gets complicated by secondary bacterial infections which can overwhelm the body's defenses, leading to severe illness and potentially fatal complications: DIC (a coagulation and bleeding disorder), severe sepsis (bacteria in blood), septic shock and multiple organ failure. This severe disease state is often exacerbated by the undernourished, underweight and immunocompromised status of many of these young patients. Most of them will simply not have the strength nor the body condition required to deal with severe disease for any great length of time (already thin puppies will waste-away with disease as it progresses).
Puppies and dogs that develop severe, progressive, neurological signs of distemper will often die or require veterinary euthanasia. This might be an immediate requirement (puppies with difficult to manage seizures) or something that occurs far down the track (e.g. as might eventually occur in an older dog showing signs of gradual brain deterioration from old-dog encephalitis).
On the flip side, animals that manage to survive the severe respiratory and/or gastrointestinal signs of distemper and which do not go on to develop severe neurological signs may do okay. These animals might be left with residual momentos of their time of illness (hard noses, hard pads, permanent dry eye, scarring of the lungs etc.), but they will be alive and their quality of life might be very good. Even some of the animals that do develop some neurological signs (distemper chorea, blindness, intermittent fits etc.) may have a good quality of life if these neurological deficits are compatible with life. They may require life-long medications to ensure that their condition remains under control.
Also on the positive side, animals which do possess some degree of immunity and which develop only mild, self-limiting respiratory or gastrointestinal signs of distemper (see section 4i) will usually do fine too.
Note - remember that it is possible for these apparently 'recovered' animals to retain low levels of distemper in their bodies (especially the brain) for many years. These animals might possibly go on to develop distemper-related diseases such as chronic, progressive dementia (old dog encephalitis) in the years to come.

8. Prevention of canine distemper - hints for the typical dog and ferret owner.
The above discussions about distemper and its grave prognosis should have made it very clear to you just how important it is that steps are taken to prevent puppies from getting this disease. Prevention is far better than cure when it comes to distemper! Prevention of distemper virus involves three key steps: immunization; avoiding contact with contaminated environments and enhancing the health, body condition and immunity of your pet animal.
1: Vaccinating against distemper.
Distemper is one of the five core vaccine viruses used in almost all puppy vaccines. Typically normal, healthy puppies receive live attenuated virus vaccines for their first and subsequent distemper vaccinations: these vaccines promote better and longer-lasting immunity (see our how vaccines work page for information on live versus killed vaccines). In the case of distemper, I have not found any evidence that killed vaccines are even still available on the veterinary market.
Vaccination against canine distemper typically begins with a first needle that is administered at 6-8 weeks of age.
Following the 6-8 week distemper shot, your puppy will require follow-up distemper vaccinations. The protocol for these follow up boosters differs depending on the type and brand of distemper vaccine used by your vet and on the manufacturers' recommendations for use. In particular, whether or not the vaccine is a conventional type of vaccine or a newer, potentiated vaccine will have a huge effect on the vaccine protocol applied. Your vet will have all of the relevant information on the vaccines s/he uses and will notify you of when the next vaccinations are due.
The original, conventional vaccines:
The original conventional vaccine brands put out by vaccine companies (and still commonly used) typically advised puppy vaccinations at 6-8 weeks, 12-14 weeks and 16-18 weeks (basically, three injections approximately one month apart). The reason for the (comparatively) long course of puppy shots was the issue of maternal immunity and the fear that, if puppies were not vaccinated at 16-18 weeks, their maternal antibodies might have 'killed off' the previous two vaccinations and thereby prevented the puppy from gaining its own protective immunity. See vaccinating the pregnant bitch for details on maternal immunity.
The newer potentiated vaccines:
More recently, potentiated vaccines have been brought out that stimulate a greater immune response, overcome maternal immunity and allow for the vaccine course to be completed earlier (by 12 weeks), thereby allowing earlier socialization. Vaccines of this type include Fort Dodge's Protech Duramune vaccine range. The vaccine guidelines for these vaccines typically advise a 6 week vaccine, 9 week vaccine and a 12 week vaccine or (if the first vaccination was an 9 week distemper shot), a 9 week and a 12 week vaccine only. A couple of the very new potentiated vaccines (e.g. Intervet's Nobivac DHP and Fort Dodge's DuramuneAdult C3) even allow for a 10-week final vaccine. With these vaccines, shots are administered at 6 weeks, 8 weeks and 10 weeks or (if the first immunization was given at 8 weeks), at 8 weeks and 10 weeks. Full protection for a year is conferred within a week of the final distemper inoculation.
The newer potentiated vaccine types also feature 'one-shot protection' in that full immunity (12 months minimum) can be attained with a single distemper vaccination if the vaccine is given at or after 12 weeks (for the 12-week finish types) or if the vaccine is given at or after 10 weeks (for the even newer 10-week finish types). This is a great feature, but owners should not wait until 10 or 12 weeks has passed before getting their puppy their first distemper needle because the animal will unprotected until that time.
Following the course of puppy vaccines, your dog will need to receive a distemper booster annually to remain fully protected. Newer vaccines such as Intervet's Nobivac DHP and Fort Dodge's DuramuneAdult C3 confer immunity against distempervirus for up to three years.
Vaccine related disease and your choice of distemper vaccines:
Generally, the choice of live vaccine type (strain of virus used in the vaccine) administered by a vet is not of any real concern to owners of young puppies. All distemper shots currently available on the veterinary market seem to be of equally good effectiveness in preventing distemper disease and the newer vaccines being introduced, are being improved all the time. The proof is in the pudding: thanks to immunization programmes is it now quite rare to see clinical cases of severe distemper in Australia (where I come from).
The main time that I would advise a bit more caution in the selection of live distemper vaccines is in the inoculation of certain lines of pure breed dogs. Certain breeds of dogs, in particular the Weimaraner, seem to be very sensitive to certain vaccine virus strains and can develop HOD or juvenile cellulitis as a result of receiving them. My advice (supported by Greene CE) to owners of Weimaraners is to get their vet to use a recombinant distemper vaccine such as Merial's Recombitek vaccine (where RNA from distemper is placed into a different, live, non-virulent type of carrier virus) or use the lower-virulence Onderstepoort strain of live vaccine. Testing antibody levels in these dogs can indicate whether the animal needs vaccination, thereby allowing distemper vaccines to only be given when the animal actually requires them. Note that recombinant vaccines may be less immunogenic and, depending on the brand, vaccination may need to continue up until 16 weeks of age.
Vaccinating ferrets against distemper:
Pet and commercial ferrets (and other suspectible domesticated mustelids - stoats, weasels etc.) also require vaccinations against distemper in order that they might be protected against the fatal disease. The live C3 vaccines (vaccines containing the three main viruses commonly vaccinated-for in dogs: parvovirus, distemper virus and adenovirus) are generally safe to use in ferrets. A 1/3 to 1/2 of a typical dog dose of vaccine tends to be given to a ferret and the vaccination schedule (timing of vaccines and when they are due) tends to be similar to that of the dog, with first vaccinations administered at 6-8 weeks of age.

2: Avoid contact with contaminated environments:
As stated in section 3 (Where do animals catch distemper from), anywhere that dogs have been (parks, vet clinics, grooming salons, dog shows) could potentially harbour infectious distemper and parvovirus organisms. Consequently, your puppy should not be taken out of your home, into the public arena and put into contact with any potentially contaminated surfaces or other animals until he or she is fully vaccinated and your vet says it is safe to socialize.
Another potential risk to your unvaccinated puppy is bringing diseases home with you. If you have visited a place where there has been distemper infection (or any outbreak of infectious disease, for that matter), don't bring the disease back to your house where your unprotected puppy can catch it! Change your clothes, disinfect your shoes and shower thoroughly (this includes washing your hair) before greeting your pet. Ideally, disinfection should take place somewhere other than your own home. The same precautions should be taken when other people visit your home: ask them if they have had any potential contact with infectious diseases.
If you have had a case of distemper in your own home and/or yard, then you will need to disinfect these contaminated areas carefully in order to make them safe for any new puppies that you bring home in the future (see section below on distemper virus decontamination). Thankfully, canine distemper is a fragile virus, which is very susceptible to many kinds of physical and chemical disinfection techniques. It should be possible to remove it from your home with thorough cleaning.
Avoiding heavily contaminated environments is still advisable once your dog has been fully vaccinated. Once immunized, your pet can go to the show, the park, beach, groomer or pretty much anywhere else, however, I would still recommend avoiding areas where there has been recent infection and illness. Vaccinated dogs that get exposed to very heavy environmental levels of distemper particles can still catch the disease and become sick.
3: Enhancing the health, body condition and immunity of the animal.
A big part of infectious disease prevention, including distemper prevention, requires the activity of a healthy, fully-functioning immune system. Although vaccination is key to promoting the 'right type' of immune response, the overall health and wellbeing of the animal is critical if there is to be a strong immune system response towards a disease. Disease prevention involves a holistic approach, with nutrition, exercise and mental health care all important parts of the process. Animals that are in good body condition and which have been given a balanced diet and are well-exercised and emotionally sound (e.g. not overly stressed or bored etc.) will generally be more resistant to disease and able to mount a better immune response.
Puppies and ferrets that are malnourished and/or which harbour other bacterial and parasitic infections in their intestines are prone to more severe distemper infections. Thus, good nutrition and control of intestinal parasites (worming etc.) and harmful bacteria (Clostridia, Salmonella etc.) are important in preventing and reducing distemper severity.
Some hints and tips:
- Puppies should be routinely wormed.
- Puppies should be fed a completely balanced (AAFCO approved) puppy diet.
- Puppies should be played with and exercised within the home until fully vaccinated (this human contact fulfills their exercise and mental health needs, but keeps them safe from disease until fully vaccine protected).
- Dogs should be walked twice daily (once vaccinated) for a bare minimum of 15-30 minutes at a time to aid both their mental health (reduces boredom) and exercise needs.
- Dogs should have toys and adequate room to move (e.g. yard size) to reduce boredom and stress whilst you are at work.
- Dogs should not be overfed or allowed to become obese.
- Purchasing in-bred animals should be avoided - excessive in breeding may result in appearance of genetic immune disorders. In the case of distemper, certain 'lines' of purebred dogs (e.g. Weimaraners) are prone to vaccine-related distemper disease.

9. Controlling distemper in high-risk and/or already contaminated environments.
Distemper outbreaks are generally quite rare these days due to improvements in vaccination schedules and environmental decontamination and disinfection techniques. Occasionally outbreaks do still occur in high-population dog breeding facilities; greyhound breeding and racing facilities; businesses which admit and/or house many dogs of varying backgrounds (e.g. veterinary clinics, grooming salons, dog clubs, dog classes) and in individual homes that have had a pet contract distemper (and are needing to make the place safe again for other dogs and new puppies).
Businesses and homes that have had an outbreak of distemper need to have plans in place to control the outbreak (prevent it from spreading to other dogs and locations) and to cleanse their facilities of the organism, so that they will be safe in the future. Control and prevention of disease in these situations involves:
1) protecting the susceptible animals and preventing them from becoming infected and
2) reducing environmental contamination and destroying the virus particles.
1: Protecting the susceptible animals.
In a situation of high distemper virus contamination of the environment, any unvaccinated or under vaccinated animals; any very young or very old animals; any unwell animals and any animals of high-risk, immunocompromised breed-lines (e.g. Weimaraners) are going to potentially be susceptible to infection. The risk of these animals contracting distemper can be reduced in the following ways (this is by all means not an exhaustive list):
1) Keep all females of breeding age up to date with vaccines.
Ensure that pregnant bitches are up to date with their vaccines so that they have some levels of maternal immunity (distemper antibodies) to pass onto their newborn puppies through their colostrum. Because of a lack of killed distemper vaccine availability, immunisation of pregnant bitches against distemper is not an option.
2) Isolate pregnant bitches and litters.
Isolate bitches in easy-to-disinfect (e.g. tiled or concrete areas, not grass or soil) pens, which have preferably never been contaminated with distemper, from the time of whelping to the time of weaning. These pens should be as far away as possible from the main dog population because distemper can spread over long distances in aerosols produced from a single cough or sneeze. If whelping bitches and pups can be removed to a new non-contaminated premises altogether, while decontamination of the distemper-infected facilities is occurring, this would be even better. All bedding and feed and water bowls provided should be new (or well-disinfected) and should be strongly disinfected after use by the bitch (most disinfectants kill CDV).
3) Ensure that puppies get their colostrum on time (<24 hours after birth).
Puppies must be monitored to ensure that they do get their colostrum (maternal immunity). Bitches that are recovering from caesarean section (unable to fed the pups yet) or that are initially reluctant to feed the pups for other reasons can be milked of their colostrum and this can be fed to them through bottle or stomach tubing.
If the bitch has no colostrum or leaks her colostrum early, plasma can be taken from the bitch and given to the puppies either orally in the milk (within the first 12-24 hours) or via plasma transfusion (if over 24 hours).
4) Don't expose puppies to contaminated environments.
Puppies should, ideally, go from the safe whelping zones straight to their new owners. The aim is to sell and get the pups out of the environment ASAP. They should not come into close contact with the general canine population where non-clinical carriers might be present (remember aerosolised virus transmission) nor any cold climate areas that are impossible to disinfect (remember that sunlight and hot temperatures should kill most environmental CDV contamination). Early weaning (4-5 weeks instead of 6+ weeks) is a consideration here - try to get the pups out of the environment as early as possible.
5) Vaccinate all animals according to vaccine company recommendations.
6) Puppies at high risk may be vaccinated 2 weekly: from 6 weeks of age until 12 weeks.
7) Wear gloves.
Whelping bitches and unvaccinated or not-fully vaccinated puppies in high risk situations should be handled with gloves (plastic disposable drapes are also available for the extra cautious to shield dogs from your possibly contaminated clothing). New gloves should be used for every litter to avoid passing CDV infectious organisms on from one bitch (and litter) to the next. If possible, gloves should be used when handling all other dogs on the premises too (though it might not be practical).
8) Avoid in breeding.
In breeding (e.g. breeding facilities) should be avoided to reduce the risk of genetic immune system disorders appearing. Weimaraners, for example, are very prone to CDV and CDV-vaccine-related disease and it is thought that in breeding and line breeding may have played a role in this problem.
9) Reduce stress.
Ensure that all animals have adequate nutrition and exercise and are kept stimulated (both mentally and physically) to reduce stress. Happy, well-nourished animals of good bodyweight generally have a better immune system and are better equipped to cope with disease. Remember to treat each animal as an individual: record the weights and body condition of each puppy or dog to ensure that the nutrition provided is adequate for him or her and to ensure that the animal is actually getting fed. It is easy in crowded situations for individual animals to be underfed (as an individual, they might simply need more food than is on offer) or for carers not to realise that a puppy is being bullied out of a meal.
Making sure that kennels and runs are warm and dry and free of draughts and chills will also go a ways to keeping animals comfortable and stress-free. Temperature control in runs is also important: excessively cold and hot conditions are stressful and can facilitate disease.
10) Control other easily-prevented diseases that might compromise an animal's gastrointestinal function, respiratory function or immune system.
Respiratory and enteric bacterial diseases and high parasite burdens are associated with a poorer response to parvo infection and logic would dictate that such pre-existing disease would probably not be helpful in cases of CDV. Chronic diseases can cause chronic, low-grade stress which may suppress the immune system response to CDV. Control of these other pathogens, through appropriate medicines and parasite programs (routine worming etc.) is vital. Good hygiene is crucial here too: ensuring that all runs, feed bowls and water dishes are cleaned promptly of fecal, vomit and urine contamination and ensuring that excrement is not permitted to spread to other runs or kennels through gutters and run-off. Most gastrointestinal organisms are spread through fecal-oral contact: less feces means less disease transmission.
11) Avoid overcrowding of animals.
Overcrowding promotes rapid infectious disease spread from animal to animal; it promotes stress which suppresses the immune response of susceptible animals and overcrowding makes it difficult for facility operators to find a place, sufficiently out of the way, to isolate the sick. With diseases like distemper, overcrowding is of particular concern because a single cough or sneeze can spread virus particles over wide distances, potentially affecting many animals.
12) Depopulate.
Distemper is one of the few diseases where complete depopulation and resting of a facility (removing all animals for a period of time) can be very effective in rendering it non-infectious. Distemper is not only very susceptible to most disinfectants (thorough disinfection of all of the premises will usually be enough to kill the virus), but it is also susceptible to heat and drying. Depopulating a premises, thoroughly disinfecting it and letting it rest, unpopulated, for a number of weeks will usually be enough to remove CDV completely, especially in warmer, drier climates. In cold climates, CDV may be more resistant to the effects of heat and desiccation, so your disinfectant job will need to much more thorough.
2: Reducing environmental contamination:
In any place where distemper has occurred, it is important to ensure that contamination is minimized where possible (e.g. reduce the amount of virus that enters the area); that the virus is destroyed as thoroughly as possible (decontamination of the environment) and to ensure that the virus does not spread from the contaminated regions to 'clean' regions of the premises and beyond. In the case of distemper, preventing contamination is actually the harder of the tasks (because distemper can travel place to place via the air and even through ducting systems), whereas decontamination is actually quite easy (because the virus is so easy to kill with modern disinfectants).
1) Reduce the incidence of shedders (non-clinical carriers of virus).
In any population where a disease process has become established, there is likely to be a subset of animals that carry the virus/infection but which do not show any outward signs of disease. These animals are the biggest problem of any disease eradication programme. Since these pets look so normal, people often do not realise that they are infected. As a result, they permit them to mix freely with other animals and have access to 'clean' regions of the premises. These animals shed infective particles of virus all over the environment, contaminating it for other animals, which might be less protected and then show disease.
Animals that carry distemper are difficult to identify. As mentioned in section 5, even identifying an animal that is sick with the disease can be really tricky. One thing we do know is that animals which have been sick from distemper (this includes animals that get the severe disease state but recover and animals that just get the mild disease symptoms of mild gastrointestinal or respiratory disease) will often shed infectious distemper particles for up to 3 months (90 days) following recovery. i.e. they will go into a carrier state after recovery. You can reduce contamination of the environment by keeping these 'recovered' distemper animals out of your premises for at least 3 months (up to 6 months to be very safe).
Vaccination can be used to improve animal immunity towards disease and reduce the incidence of carriers. In the case of distemper, vaccination is not 100% in preventing transient carrier states from developing. It is thought that a lot of vaccinated animals may develop subclinical infections with distemper and shed virus for a short period of time without owners being aware of the infection. Still, every little bit helps. It is partly for this reason (not just preventing animals from becoming clinically unwell) that ALL animals in any breeding or multi-dog facility must be fully vaccinated and kept up to date with vaccinations.
Animals with neurological signs of distemper only do not shed virus and are generally not infectious to other creatures.
2) Isolation of infected or sick animals.
Sick animals should be removed from the general population and put into a quarantine region (typically severely affected pets will go to the vet and the vet will isolate them in a special 'iso' - isolation - ward.) This quarantine region should not be near any thoroughfares (places where animals and people frequently walk) and well out of the way. Because of the potential spread of distemper through the air in coughs and sneezes, quarantine should ideally be off the main premise altogether and not share any air conditioning or ducting passages with animal-populated areas.
Animals in quarantine should be handled as little as possible (though not infrequent enough that they aren't getting proper care). When handled, the carer should wear disposable gloves; a disposable gown and even a hair net and goggles (many respiratory-spread pathogens can sit in your hair and within your nasal tract and mucous membranes for a period of time). All materials used by the carer should be disposed of in bins present in the iso ward so that nothing that is potentially infectious gets brought out into the 'clean' areas. Shoes are generally washed thoroughly in disinfectant foot baths as the carer leaves the isolation areas - this should be enough to kill distemper particles.
3) Quarantine areas where sick animals have been.
Areas where sick animals have been should be quarantined until thoroughly disinfected (see section 12). Distemper is easily killed by disinfectant and so disinfecting the affected regions and 'spelling them' (depopulating them of animals) for a few weeks is often enough to remove all traces of virus.
4) Discard contaminated bedding.
Any towels or bedding that the sick animal has been on should be discarded as garbage once soiled. In the case of distemper, you could disinfect and salvage them if you really need them (e.g. if the bedding is really expensive or valuable), but the best option is always to throw out potentially infectious items which could harbour virus particles.
5) Be mindful of run-off and air-passages.
Be careful that run-off from quarantined areas does not travel to 'clean' areas. Be mindful of gutters and also gaps under the walls of pens, that might allow faeces, vomitus or urine from infected animals to contaminate clean areas or waterways. Be aware of the potential of distemper to spread via the air through air conditioning or heating ducts and across open spaces.
6) Ensure good hygiene with urine, feces and vomitus.
Even among the 'apparently non-infected' canine population, it is always best that the faeces and urine from one animal not be allowed to contact other animals. This is just good hygiene and reduces the risk of all manner of diseases spreading between animals.
7) All infected rooms, pens and fomites (feeding dishes, grooming gear, benches etc.) should be disinfected thoroughly. Information on distemper disinfection is contained in section 10.
8) Avoid overcrowding of animals.
Overcrowding promotes rapid infectious disease spread from animal to animal; it promotes stress which suppresses the immune response and overcrowding makes it difficult for facility operators to find a place, sufficiently out of the way, to isolate the sick.
9) Consider your choice of surfaces.
It is almost impossible to keep infectious diseases and parasites out of dirt flooring and grassy areas: such surfaces are difficult to decontaminate and they tend to pool water, which promotes growth of infectious organisms. In the case of distemper control, surface choice is not as important as it is with, say, parvovirus. Even if you can not get at the area with disinfection, distemper particles will usually die off within hours to weeks if exposed to heat (especially heat over 20C), sunlight (UV light) or drying conditions (desiccation).
I make mention of surface choice here mostly because of other, more resistant, diseases such as parvo (which don't simply die off in the sun) and because of relative ease of distemper contamination. Sure, distemper may die in the sun, but this takes time. It is far quicker and easier to rid yourself of distemper if you can thoroughly disinfect your premises top to tail. For ease of disinfection (including parvo etc.) you are better to go with cement or tile flooring, which can be easily cleaned of feces, urine and vomit and readily disinfected.
Routine hygiene and cleaning is a must in all dog facilities. All surfaces (even ones without distemper) should be routinely disinfected and kept clean. Feces and urine must be removed daily. Routine spraying of runs with water to remove particulate matter is important (these harbour infectious organisms and bacteria) and intermittent (weekly to 2-weekly) steam-cleaning of surfaces is useful (parvo is killed by steam-cleaning).
Don't forget to clean cage or door bars and vertical walls where a dog might have sneezed!
10) New animals should be quarantined.
As a routine part of infectious disease prevention, all new dogs to a breeding facility should be quarantined away from the rest for at least a month. They should be fully wormed and vaccinated and monitored for disease appearance. Only when the time is up and the animal considered free from disease, should he or she be allowed into the greater population.
Note that this quarantine zone should not be an area that has had diseased animals in it before. If it is, the new non-diseased dog could contract disease from the quarantine area.
Quarantined animals should be treated like isolation animals, with gloves, gowns and foot bathing (or shoe covers etc) used to prevent disease going from quarantine into the rest of the population or from the rest of the population into the quarantine zone.
In theory, households looking to introduce new animals into their already existent pet family could also employ a similar quarantine procedure. If this is not possible or practical, new additions to the family should ideally be bought from reputable breeders or families (places with no history of distemper and excellent standards of pet care and hygiene) and vaccinated and wormed prior to arrival.
11) Staff should know the signs of unwellness and distemper infection in puppies.
Early detection of illness is key to establishing rapid isolation of the animal and reducing spread of diseases like distemper. Remember that it takes up to 6 days for distemper to begin shedding in feces, urine and nasal secretions and puppies often show some signs of unwellness before this. Staff should look out for lethargic, inappetent (or reduced appetite puppies) or 'loner' (puppies on their own) puppies. Puppies with any vomiting or diarrhea should be immediately isolated until tests provide a diagnosis (remember that distemper diagnosis can be difficult). Recognition of puppies in poor condition or unwell condition is very important in places like pet shops that receive lots of unvaccinated puppies through their doors. These places should not take on any weak or sickly puppies to sell, as they risk contaminating their facilities and all other healthy pups that they get through.
12) Good record keeping.
Breeders that receive dogs from elsewhere and pet shops that receive lots of for-sale puppies from various sources must keep good records of where these animals have come from. Good record keeping allows these facilities to recognise breeders and sellers that are frequent offenders and who frequently sell underweight, malnourished, wormy or distemper-affected animals. Once identified, not buying from such places can go a big way towards preventing distemper and other contagions from getting into your facilities.
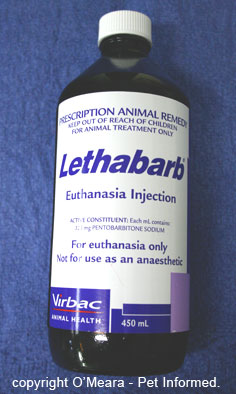 13) Euthanasia of distemper cases.
13) Euthanasia of distemper cases.
In some situations where isolation or quarantine is difficult to maintain (either due to space or staffing reasons) and the sheer number of dogs or condition of the dogs (e.g. numerous unvaccinated puppies; puppies with poor nutritional state, high parasite burdens and high levels of stress) makes spread of disease highly likely, euthanasia of clinically affected animals may be the best way of managing the disease. This is certainly the case in many dog rescue shelters (strays brought in with distemper are generally euthanased on suspicion), but it may even apply to some breeding facilities that are in the process of trying to control an outbreak. In these situations, control of disease may be more readily achieved by euthanasing the sick, depopulating the healthy to clean zones and disinfecting and spelling the contaminated facility for a few weeks, prior to bringing the well animals back again.
14) Control rodents and insects.
Rodents and insects can potentially carry distemper organisms on their feet from animal to animal and place to place. Strict control of these vectors must be put into place in order to reduce the spread of distemper in a facility. Obviously, removal of factors which attract rodents (such as grass, grain, open dog-food packs and warm, hidden areas to breed) and flies (feces, open foodstuffs) is vital, but adequate control may need to include the use of rodent poisons and insecticides and 'fly traps'.

10. How to disinfect the environment following distemper contamination.
Regardless of whether an affected distemper case appears in your own home or in a larger multiple-dog environment such as a breeding facility or veterinary clinic, it is important that correct hygiene measures are taken to clean and disinfect the contaminated areas. Fortunately, distemper is really easy to kill and there are many ways (both chemical and physical) to remove the organism from surfaces and fomites (feed bowls, water dishes) in order to prevent the disease from spreading.
Chemical agents (disinfectants) used to kill distemper virus.
Initial cleaning with water.
Before a disinfectant can be used on an area, it is important to thoroughly scrub the area with water beforehand. This is to remove gross fecal, urine, vomit and soil matter from the surfaces. It is important to do this because organic matter such as feces can inhibit the effects of some disinfectants (for example QUATs) and even deactivate them! Removing fecal and soil matter will also reduce the surface area over which the distemper particles can hide out, thereby enhancing the ability of the disinfectant to make contact with them.
This initial cleaning process should not contain disinfectants or other soaps because some disinfectants will react badly with or deactivate other kinds of disinfectants (the reaction can even create poisonous gasses which you might breathe in).
Quaternary ammonium compounds (QUATs).
These substances (also termed cationic disinfectants or cationic surfactants) are probably the most common disinfectant substances used by most households today. They are readily available and work well in the killing of CDV.
Although no disinfectant can be termed safe (they all have nasty poison warning labels on their packets), the quaternary ammonium compounds are probably the most innocuous of the chemicals that will be mentioned on this page. They can be used to mop over floors, clean gutter, wipe vertical surfaces and are frequently placed in foot baths. A lot of the detergents used to wash clothes (e.g. fabric softeners and washing powders/liquids) are quaternary ammonium compounds: they should be fine to remove CDV from clothing and bedding.
There are many kinds of QUATs available for household or commercial use, including dodecyl dimethyl ammonium chloride, N-alkyl dimethyl benzyl ammonium chloride and benzalkonium chloride. Of these, benzalkonium chloride is the more common. Used at a concentration of around 0.3%, it readily kills CDV organisms. The most important thing to remember, when using benzalkonium chloride or any of the QUATs , is that these disinfectants are deactivated by organic matter and other soaps and detergents. Therefore, a thorough clean (water and scrubbing) of the CDV contaminated area before use is important.
Like many disinfectants, QUATs have the ability to cause chemical burns to skin, mouths, eyes and delicate mucous membranes and open wounds. They need to be thoroughly rinsed from any surface and/or fomite after application so that animals are not able to ingest them or get burned by them. QUATs (like any disinfectant chemical) should ideally only be used in well-ventilated areas or, if used in poorly ventilated areas, be used with appropriate safety apparatus (face and eye masks, possibly even breathing apparatus).
For those of you looking for effective, biodegradable, non-toxic chemicals effective against CDV, there is a new compound put out by the Nutribiotic company called Citricidal (ref. Greene CE). This is a natural diphenol derived from grapefruit seed.
Phenolic compounds.
The phenolic compounds would probably be equal to the QUATs as my ideal choice of CDV-killing disinfectant compounds. Similar to the QUATs, they have a nice balance of effectiveness and human and animal safety (remember, no disinfectant chemical could ever be termed 100% safe, but the QUATs and phenols are probably a bit nicer to use than many of the chemicals discussed further down this page.) Phenol at 0.75% concentration has been found to kill off enveloped viruses such as CDV. Phenols are of particular use in kennelling situations since they are not deactivated by other soaps or organic soil and faecal matter. Like most of the disinfectants discussed on this page, phenolic compounds can leave skin and mucous-membrane irritant residues and surfaces cleaned with them should be rinsed thoroughly after application.
For those of you looking for effective, biodegradable, non-toxic chemicals effective against CDV, there is a new compound put out by the Nutribiotic company called Citricidal (ref. Greene CE). This is a natural diphenol derived from grapefruit seed.
Aldehydes.
 Aldehyde chemicals such as formaldehyde (formalin) and glutaraldehyde and other closely related substances are high-level disinfectants which are able to kill distemper organisms, even at very low concentrations (formalin at around 0.5% concentration is effective). Available as liquid disinfectants or as gasses, these chemicals are often used in the sterilization of sensitive optical equipment and equipment that is sensitive to heat and other chemicals. Of the two forms, the liquid forms, particularly formaldehyde, are readily available and are able to be used on premises to kill CDV.
Aldehyde chemicals such as formaldehyde (formalin) and glutaraldehyde and other closely related substances are high-level disinfectants which are able to kill distemper organisms, even at very low concentrations (formalin at around 0.5% concentration is effective). Available as liquid disinfectants or as gasses, these chemicals are often used in the sterilization of sensitive optical equipment and equipment that is sensitive to heat and other chemicals. Of the two forms, the liquid forms, particularly formaldehyde, are readily available and are able to be used on premises to kill CDV.
I would suggest getting professional advice if considering using formaldehyde or one of its relatives to disinfect for CDV. Compared, say, to the quaternary ammonium compounds, these substances are really nasty. Effective, but nasty. Formalin releases noxious vapors that irritate the airways and nasal passages and it is a highly carcinogenic (cancer causing) substance. Aldehydes should ideally only be used in well-ventilated areas or, if used in poorly ventilated areas, with appropriate safety apparatus (face and eye masks, possibly even breathing apparatus). Once applied and given time to act, aldehydes must be rinsed thoroughly, leaving no residues, and the area allowed to ventilate well before animals can be reintroduced. Given the choice, if it was me, I would stick with the QUATs.
 Bleach.
Bleach.
A simple, readily available solution, bleach made up in water to a 1:30 solution (1 part bleach: 30 parts water) will kill parvo and most enveloped viruses such as CDV. The solution must be applied thoroughly to ALL contaminated surfaces and left on for at minimum of 10 minutes to be effective.
Be aware, of course, that some surfaces and materials will not tolerate bleach (it is corrosive at high concentrations). Also be aware that bleach is not safe to breathe in (there are lots of warnings on the labels). The bleach solution should ideally only be used in well-ventilated areas or, if used in poorly ventilated areas, with appropriate safety apparatus (face and eye masks, possibly even breathing apparatus). Once applied and given time to act, the bleach must be rinsed thoroughly, leaving no residues, and the area allowed to ventilate well before animals can be reintroduced to the area. If it is not rinsed away well, bleach can cause severe ulcers to the skin and mouths of animals that walk on or lick it.
Ethylene Oxide.
This is a powerful gaseous chemical which is able to kill most infectious disease organisms. It is generally only available in hospitals to sterilize equipment, however, it could potentially be applied to contaminated canine fomites (dog feed bowls, grooming gear) in order to kill distemper virions. I would consider it to be too cost prohibitive and equipment intensive to be a real practical consideration for the average dog breeder or householder. Besides, there are perfectly effective, more readily available, cheaper options available for killing off CDV.
Other chemicals and antiseptics that may be effective against CDV.
Chlorhexidine and povidone-iodine (betadine) are two of the antiseptic disinfectants commonly used in veterinary hospitals to flush wounds and to prepare skin for surgery. At normal concentrations (e.g. 0.5% up to 10% for betadine), chlorhexidine and povidone-iodine have the potential to kill CDV, provided that enough contact time is allowed for the substances to do the job. As far as their effectiveness as room-cleaners goes, betadine can be deactivated by organic materials (feces, vomit etc) and soaps, whereas chlorhexidine is more resilient towards these factors. Both have the potential to stain surfaces (especially betadine, which stains surfaces yellow). In reality, chlorhexidine and povidone-iodine were not really intended for room-disinfectant purposes. These are great skin and wound antiseptics (the mainstay of surgeries everywhere), but they are not practical for decontamination of a premises: there are better cleaning agents (e.g. QUATs) available for this purpose.
Chloroform and ether are two other compounds that have been found to kill CDV, although their availability, safety and practicality are highly questionable. Chloroform, for example, is a potential anaesthetic agent (not safe for you to be breathing in during routine decontamination). I would steer clear of these in favour of the QUATs.
Non-chemical agents used to kill distemper.
Steam-cleaning.
Enveloped viruses such as distemper are not resistant to intense heat and pressure. Steam cleaning will kill CDV and even parvo virus organisms and may be an option for carpets, clothing and bedding where other chemical compounds might not be appropriate. Autoclaving (whereby hospitals and vet clinics use intense pressure and heat to sterilize surgical equipment) is a good way of removing infectious distemper organisms from steel fomites, instruments and cloth materials.
When using steam to kill off infectious organisms, it is important that adequate temperatures be achieved, that adequate pressures be achieved and that adequate contact time is maintained. In the case of CDV, any temperature in excess of 50C for half an hour will kill it. Most steam cleaners and autoclaves go well in excess of 50C and the time taken to kill the organism is much less.
Depopulation and resting the environment.
Sunlight, heat and dry, desiccating conditions all kill distemper. Thus, simply waiting can be a nice, chemical-free way of removing CDV from a contaminated environment. In most regions where temperatures exceed 20C, Distemper virus organisms will be deactivated in a few days provided they are exposed to this temperature or greater (in reality, the virus probably deactivates within hours, but if you can be patient and allow the environment to rest for a couple of days to a couple of weeks, this will give you a better margin of safety - this is why I suggested depopulating for a few weeks in section 9). In cold climates (close to freezing), distemper can last for quite a few weeks and so you are either going to have to wait and rest the area longer or rely more on chemical disinfection.
Remove the infected surfaces.
This is an expensive way to remove infectious disease organisms, however it does work. Routinely replacing gravel, topsoil or lawn surfaces that have become contaminated and replacing them with new, fresh, non-contaminated surfaces is an excellent way to remove infectious disease organisms. If the difficult-to-clean infectious surfaces (soil, lawn etc) can be replaced with a new, easy-clean surface such as concrete or tiles or metal (in the case of runs and cages), so much the better. In the case of CDV, particularly in warm climates, replacing of surfaces is probably overkill. The virus is easy to kill with basic disinfectants and will also deactivate in sunlight, heat and drying conditions.

11. Summary and take home messages:
Puppies and adult dogs which are unvaccinated or under vaccinated or which have immune system disorders are at risk of contracting distemper if they are taken out into public places or allowed to meet other animals. Particular high-risk environments can include indigenous people's camps, lower socioeconomic suburbs, some breeding facilities and some pet shops and vet clinics.
Clinical distemper disease is not commonly diagnosed in Australia due to the success of vaccination protocols and the virus's short-lived existence in the environment (particularly in hot, dry environments such as Australia).
The virus only lasts a short time in most environments with temperatures over 20C and it is very susceptible to most household disinfectants and chemicals. The virus can persist for longer (weeks) in cold climates, approaching freezing point (0 degrees C).
The signs of distemper vary from animal to animal, but can include: gastrointestinal signs
(vomiting, bloody (hemorrhagic) diarrhea, watery or mucoid diarrhoea, abdominal pain); respiratory signs (pneumonia, coughing, sneezing, nasal and eye discharges); neurological signs; skin disease signs (hard pads, hard nose pustules etc.); bone signs (HOD, lameness and arthritis); eye disease and dehydration, anorexia and fever.
Neurological signs are often progressive and frequently fatal and they can appear after the other nasty disease signs (intestinal signs, respiratory signs) have resolved.
Distemper is an expensive; sometimes difficult and often unrewarding disease to treat. Puppies will need to be kept in isolation at a vet clinic and placed on intravenous fluids and various medications. Ongoing treatment and monitoring is very costly.
Many severely affected puppies will die from overwhelming secondary bacterial infections or CDV-associated neurological diseases, despite what we do.
Insurance companies may not cover the cost of this treatment - most exclude vaccine-preventable diseases, such as distemper, from their coverage.
Prevention is definitely the best form of treatment. Prevention is achieved by vaccinating dogs and ferrets against the disease and controlling where the animal is allowed to go (particularly when it is not fully vaccinated).
Some breeds of dogs (Weimaraners) may show disease with certain live CDV vaccines and so they need to be vaccinated with more caution with regard to type and brand of vaccine.
In high risk distemper situations, complex plans of facility management and new protocols (e.g. vaccine protocols, isolation protocols, quarantine protocols, cleaning and disinfection protocols) may need to be put into place to reduce the spread of disease.

To go from this distemper page to the homepage, click here.

References and Suggested Readings:
1) Prevention of Infectious Diseases. In Nelson RW, Couto CG, editors: Small Animal Internal Medicine, Sydney, 1998, Mosby Inc.
2) Polysystemic Viral Diseases. In Nelson RW, Couto CG, editors: Small Animal Internal Medicine, Sydney, 1998, Mosby Inc.
3) Encephalitis, Myelitis and Meningitis. In Nelson RW, Couto CG, editors: Small Animal Internal Medicine, Sydney, 1998, Mosby Inc.
4) Greene CE, Immunoprophylaxis. In Greene CE, editor: Infectious Diseases of the Dog and Cat, St. Louis, 2006, Saunders Elsevier.
5) Greene CE, Appel MJ, Canine Distemper. In Greene CE, editor: Infectious Diseases of the Dog and Cat, St. Louis, 2006, Saunders Elsevier.
6) Greene CE, Environmental Factors in Infectious Disease. In Greene CE, editor: Infectious Diseases of the Dog and Cat, St. Louis, 2006, Saunders Elsevier.
7) Greene CE, Prevention and Management of Infection in Kennels. In Greene CE, editor: Infectious Diseases of the Dog and Cat, St. Louis, 2006, Saunders Elsevier.
8) Hoskins JD, Canine Viral Diseases. In Ettinger SJ, Feldman EC, editors: Textbook of Veterinary
Internal Medicine, Sydney, 2000, WB Saunders Company.
9) General Characteristics and Classification of Viruses. In Carter GR, Chengappa MM, Roberts AW editors: Essentials of Veterinary Microbiology, USA, 1995, Williams and Wilkins.
10) Immunotherapy. Wroth O, editor: MIMS IVS Annual, St Leonards, 2001, Havas MediMedia.
11) Immunotherapy. Wroth O, editor: MIMS IVS Annual, St Leonards, 2004, Havas MediMedia.
12) Information on DuramuneAdult C3 taken from information provided by Fort Dodge Australia Pty Limited, 2007.
13) Information on Nobivac DHP and Nobivac KC taken from information provided by Intervet Australia Pty Limited, 2007.
14) http://en.wikipedia.org/wiki/Paramyxoviridae - Paramyxovirus.
15) Hunt R, RNA Virus Replication Strategies. Hunt R, editor: Microbiology and Immunology Online - http://pathmicro.med.sc.edu/mhunt/RNA-HO.htm, University of South Carolina, 2007.
16) Manzo U, Karunanidhi K, Paramyxovirus. Manzo U, Karunanidhi K, editors:
http://www.stanford.edu/group/virus/paramyxo/2005/index.htm, 2005.

Pet Informed is not in any way affiliated with any of the companies whose products
appear in images or information contained within this article. The images, taken by Pet Informed, are only used in order to illustrate certain points being made in the article.
Copyright March 22, 2008, www.pet-informed-veterinary-advice-online.com.
All rights reserved, protected under Australian copyright. No images or graphics on this Pet Informed website may be used without written permission of their owner, Dr. O'Meara BVSc (Hon).
Duramune, Protech and Fort Dodge are registered trademarks of Wyeth and its affiliates.
Companion C3 and Nobivac are registered trademarks of Intervet.
Recombitek is a registered trademark of Merial.
Dexason is a registered trademark of Ilium Veterinary Products.
Solu-Delta-Cortef and Solu-Medrol are registered trademarks of Pfizer.
Lethabarb is a registered trademark of Virbac Pty Ltd.
The Vitamin B1 and Vitamin C Injections pictured are products of Nature Vet.
Zantac is a registered trademark of GlaxoSmithKline.
Hypnovel is a registered trademark of Roche.
Metrin and Pamlin are registered trademarks of Parnell Laboratories Pty Ltd.
Baytril is a registered trademark of Bayer Australia Ltd.
The formaldehyde compound shown is a product of Cattlekare.
White King is a registered trademark of Sara Lee.
Citricidal is a trademark of the Nutribiotic company.
Please note: the aforementioned puppy vaccination schedules, adult dog vaccination
guidelines, pregnancy vaccination guidelines and information on the new immunization schedules now being made available are general recommendations only.
The information provided is based on published information and recommendations made available from the vaccine companies themselves; relevant veterinary literature
and publications and my own experience as a practicing veterinarian.
The advice given is appropriate to the vast majority of pet owners however, given
the large range of vaccine types and protocols now available, owners should take it upon themselves to ask their own veterinarian what vaccination schedules s/he is using so as
to be certain what to do. Owners with specific circumstances (high distemper virus
contamination in their environment, Weimaraners, pregnant bitches, breeders, animals on immune-suppressant medicines etc. etc.) should ask their vet what the safest and
most effective protocol is for their situation.
Any dose rates mentioned on these pages should be confirmed by a vet. Dosing rates for common
drugs are being changed and updated all the time (e.g. as new research comes in and as drug
formulations change) and information here may not remain current for long. What's more, although we try very hard to maintain the accuracy of our information, typos and oversights do occur. Please check with your vet before dosing any pet any medication or drug.
 The information contained within this article covers a range of canine distemper topics written to fully educate pet owners about distemper virus in dogs (ferrets are also discussed). The canine distemper information presented here is detailed (but still easy to understand) because we are aiming to educate owners thoroughly and provide them with enough information that they might be better informed and able to troubleshoot problems with their own pets. The topics are covered in the following order:
The information contained within this article covers a range of canine distemper topics written to fully educate pet owners about distemper virus in dogs (ferrets are also discussed). The canine distemper information presented here is detailed (but still easy to understand) because we are aiming to educate owners thoroughly and provide them with enough information that they might be better informed and able to troubleshoot problems with their own pets. The topics are covered in the following order: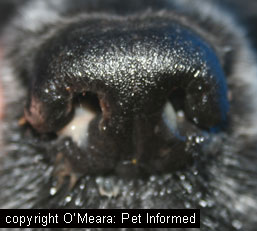 Typically, canine distemper virus affects the lymphatic system, nervous system, lungs, gastrointestinal tract,urinary tract, eyes and skin of the animal and, as a result, animals generally present with a range of neurological signs, respiratory signs, gastrointestinal signs (vomiting, diarrhea), ocular signs and skin signs. Canine distemper affected animals will also present with non-specific signs of illness: fever, lethargy, inappetence and dehydration. Occasionally, distemper can even affect other, less typical, areas of the body such as the eyes and bones and the appearance of some odd clinical syndromes such as 'dry eye', uveitis (inflammation inside the eye) and HOD (hypertrophic osteodystrophy) can result. All of these symptoms are discussed in section 4 of this article. Importantly, it must be mentioned that not every case of canine distemper presenting to a veterinarian will display all of these organ symptoms at once. Some cases show all of the signs; some only present with respiratory symptoms and some cases might show just neurological signs and nothing else. Some animals show no signs at all (they are subclinically affected). The difference in signs may reflect differences in immunity of the animals and/or differences in the strains of canine distemper in the environment (some strains are very aggressive and prefer to invade the brain, for example).
Typically, canine distemper virus affects the lymphatic system, nervous system, lungs, gastrointestinal tract,urinary tract, eyes and skin of the animal and, as a result, animals generally present with a range of neurological signs, respiratory signs, gastrointestinal signs (vomiting, diarrhea), ocular signs and skin signs. Canine distemper affected animals will also present with non-specific signs of illness: fever, lethargy, inappetence and dehydration. Occasionally, distemper can even affect other, less typical, areas of the body such as the eyes and bones and the appearance of some odd clinical syndromes such as 'dry eye', uveitis (inflammation inside the eye) and HOD (hypertrophic osteodystrophy) can result. All of these symptoms are discussed in section 4 of this article. Importantly, it must be mentioned that not every case of canine distemper presenting to a veterinarian will display all of these organ symptoms at once. Some cases show all of the signs; some only present with respiratory symptoms and some cases might show just neurological signs and nothing else. Some animals show no signs at all (they are subclinically affected). The difference in signs may reflect differences in immunity of the animals and/or differences in the strains of canine distemper in the environment (some strains are very aggressive and prefer to invade the brain, for example). 


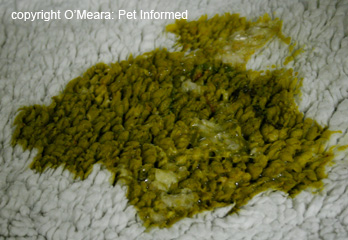 The death of the cells lining the small intestine results in ulceration and bleeding of the intestinal wall, damage which is compounded by the effect of digestive enzymes and bacterial toxins that can further erode the unprotected areas. The severe, diffuse injury of the intestinal lining results in massive inflammation (infiltration of inflammatory cells and proteins into a region of damage) of the gut. The intestine becomes swollen and paralyzed (unable to move) and a condition called ileus (non-moving gut) occurs, which results in vomiting and an inability to keep any food or fluids down. The ulceration, bleeding and massive inflammatory response that occurs in the intestines results in an enormous loss of water and body-proteins into the intestines: these are lost as diarrhea (which can be bloody, watery or mucussy) and vomit. This loss of fluids and proteins is further compounded by the inability of the animal to keep water or food down (due to vomiting) and by the fact that the nutrient-absorbing cell-lining has been lost (there are no cells left to absorb any of the food or water that does make it to the gut). The result is a massive net loss of body proteins (albumin, in particular) and massive dehydration (loss of water), which, if left untreated, will lead to shock and death.
The death of the cells lining the small intestine results in ulceration and bleeding of the intestinal wall, damage which is compounded by the effect of digestive enzymes and bacterial toxins that can further erode the unprotected areas. The severe, diffuse injury of the intestinal lining results in massive inflammation (infiltration of inflammatory cells and proteins into a region of damage) of the gut. The intestine becomes swollen and paralyzed (unable to move) and a condition called ileus (non-moving gut) occurs, which results in vomiting and an inability to keep any food or fluids down. The ulceration, bleeding and massive inflammatory response that occurs in the intestines results in an enormous loss of water and body-proteins into the intestines: these are lost as diarrhea (which can be bloody, watery or mucussy) and vomit. This loss of fluids and proteins is further compounded by the inability of the animal to keep water or food down (due to vomiting) and by the fact that the nutrient-absorbing cell-lining has been lost (there are no cells left to absorb any of the food or water that does make it to the gut). The result is a massive net loss of body proteins (albumin, in particular) and massive dehydration (loss of water), which, if left untreated, will lead to shock and death.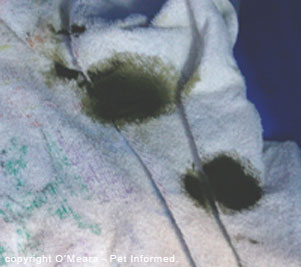





 - distemper uveitis (inflammation within the eye itself) - the surface of the cornea (clear part of the eye) will become cloudy in appearance; the pupil will shrink to a small size and the sclera (white of the eye) will become inflamed and red. The eye will be painful and the animal will squint. Left untreated, the inflammation within the eye can damage it permanently and secondary complications such as glaucoma may occur that can make the animal permanently blind.
- distemper uveitis (inflammation within the eye itself) - the surface of the cornea (clear part of the eye) will become cloudy in appearance; the pupil will shrink to a small size and the sclera (white of the eye) will become inflamed and red. The eye will be painful and the animal will squint. Left untreated, the inflammation within the eye can damage it permanently and secondary complications such as glaucoma may occur that can make the animal permanently blind. 
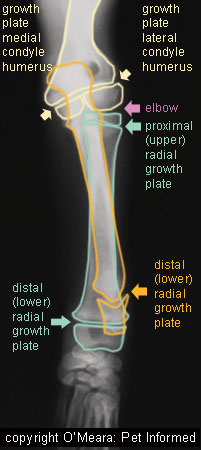
 As mentioned in section 4a, the distemper virus has certain proteins and molecules present on its surface membrane (envelope) which allow it to attach-to and invade certain cells of the animal body. These surface proteins/molecules are not only present on the membrane of the virus itself, but they are also secreted onto the surface of any dog cell membrane that happens to be invaded by the virus. These surface proteins and molecules (termed antigens) of the distemper virus are the regions of the virus that are targeted by distemper-specific antibodies of the canine immune system. For a great explanation of antibodies: how they are created and what they do, visit our
As mentioned in section 4a, the distemper virus has certain proteins and molecules present on its surface membrane (envelope) which allow it to attach-to and invade certain cells of the animal body. These surface proteins/molecules are not only present on the membrane of the virus itself, but they are also secreted onto the surface of any dog cell membrane that happens to be invaded by the virus. These surface proteins and molecules (termed antigens) of the distemper virus are the regions of the virus that are targeted by distemper-specific antibodies of the canine immune system. For a great explanation of antibodies: how they are created and what they do, visit our  There is no easy remedy or cure for distemper virus. No antiviral medication has yet been produced or made available in any mainstream capacity that will kill this organism. Consequently, the treatment of canine distemper infection is pretty much a treatment of symptoms. The aim of therapy is to keep the animal stable, and to manage and prevent any secondary complications, in the hope that the animal's own immune response will take over and destroy the disease before it does any irreversible damage (e.g. severe brain damage). The treatment options for distempervirus, their mechanisms of action and their pros and cons are discussed below.
There is no easy remedy or cure for distemper virus. No antiviral medication has yet been produced or made available in any mainstream capacity that will kill this organism. Consequently, the treatment of canine distemper infection is pretty much a treatment of symptoms. The aim of therapy is to keep the animal stable, and to manage and prevent any secondary complications, in the hope that the animal's own immune response will take over and destroy the disease before it does any irreversible damage (e.g. severe brain damage). The treatment options for distempervirus, their mechanisms of action and their pros and cons are discussed below.


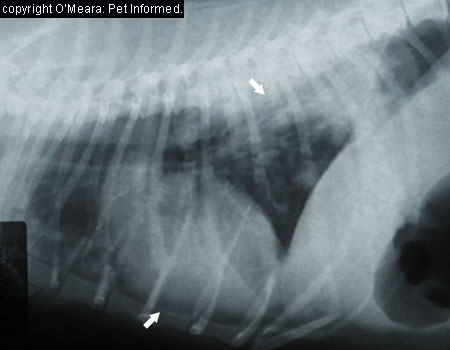
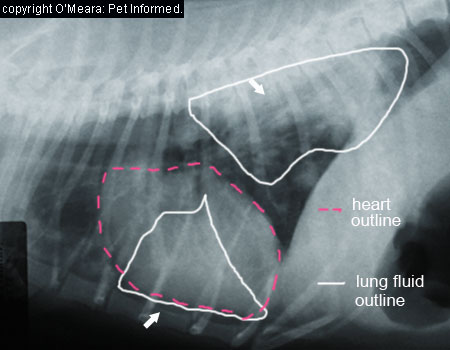

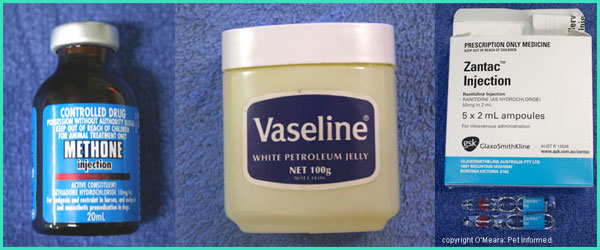


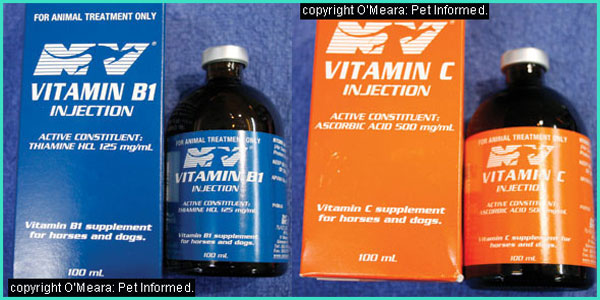
 Animals which recover from distemper to the point of being able to go home may have persistent issues (such as blindness or intermittent seizures) which require you to implement an environmental control strategies within your own house. Blind animals, for example, will usually be able to get around fine with time, so long as you take care not to move your furniture around (they end up navigating by smell and by memory); keep clutter out of their way and keep them from accessing places where they might fall and hurt themselves (steps, pools, holes etc). Animals prone to intermittent seizures should, likewise, be kept away from places where they might hurt themselves, should a fit occur. Swimming pools, steps, high verandahs and balconies are probably the biggest risks.
Animals which recover from distemper to the point of being able to go home may have persistent issues (such as blindness or intermittent seizures) which require you to implement an environmental control strategies within your own house. Blind animals, for example, will usually be able to get around fine with time, so long as you take care not to move your furniture around (they end up navigating by smell and by memory); keep clutter out of their way and keep them from accessing places where they might fall and hurt themselves (steps, pools, holes etc). Animals prone to intermittent seizures should, likewise, be kept away from places where they might hurt themselves, should a fit occur. Swimming pools, steps, high verandahs and balconies are probably the biggest risks. 

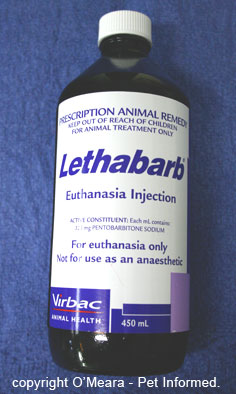 13) Euthanasia of distemper cases.
13) Euthanasia of distemper cases.  Aldehyde chemicals such as formaldehyde (formalin) and glutaraldehyde and other closely related substances are high-level disinfectants which are able to kill distemper organisms, even at very low concentrations (formalin at around 0.5% concentration is effective). Available as liquid disinfectants or as gasses, these chemicals are often used in the sterilization of sensitive optical equipment and equipment that is sensitive to heat and other chemicals. Of the two forms, the liquid forms, particularly formaldehyde, are readily available and are able to be used on premises to kill CDV.
Aldehyde chemicals such as formaldehyde (formalin) and glutaraldehyde and other closely related substances are high-level disinfectants which are able to kill distemper organisms, even at very low concentrations (formalin at around 0.5% concentration is effective). Available as liquid disinfectants or as gasses, these chemicals are often used in the sterilization of sensitive optical equipment and equipment that is sensitive to heat and other chemicals. Of the two forms, the liquid forms, particularly formaldehyde, are readily available and are able to be used on premises to kill CDV.  Bleach.
Bleach.